ENT Emergency
Epistaxis
Causes of epistaxis MANAGEMENT
Local: ( T I 3N E A V D )
• Trauma
– Nose picking
– Facial injury
– Foreign body
• Idiopathic
• Inflammation
– Infection
– Allergic rhinosinusitis
– Nasal polyps
• Iatrogenic
– Surgery (for example, ENT/maxillofacial/ophthalmic)
– Nasal apparatus (for example, nasogastric tube)
• Neoplasia
– Benign (for example, juvenile angiofibroma)
– Malignant (for example, squamous cell carcinoma)
• Environmental:
– Dry cold conditions (presentations increase during winter
– Prolonged inhalation of dry air (Oxygen)
• Anatomical
– DNS/ septal spur
– Septal perforations
• Vascular
– Congenital (for example, hereditary haemorrhagic telangiectasia)
– Acquired (for example, Wegener’s granulomatosis)
• Drugs
– Nasal sprays (for example, topical decongestants)
– Abuse (for example, cocaine)
Systemic: (HO2D)
• Haematological
– Coagulopathies (for example, haemophilia)
– Thrombocytopenia (for example, leukaemia)
– Platelet dysfunction (for example, Von Willebrand’s disease)
• Organ failure
– Uraemia —> coagulopathy
– Liver (for example, cirrhosis) —> reduced vitamin K —> coagulopathy
• Drugs
– Anticoagulants (for example, heparin, warfarin)
– Antiplatelet (for example, aspirin, clopidogrel)
• Others
– Atherosclerosis
– Hypertension
MANAGEMENT
1. Attend immediately
2. Assess patient’s ABCDE
Airway:
• Risk of airway obstruction from blood in the posterior pharynx, or decreased level of consciousness from hypovolaemia.
Breathing:
• Assess depth of breathing and respiratory rate,
• Provide high flow oxygen via non rebreather mask
Circulation:
• Assess heart rate, blood pressure and capillary refill
• Insert x2 large bore IV, check HB, cross match blood, and start fluid resuscitation
Disability:
• Monitor patients level of consciousness this help determine the severity of haemorrhage
Exposure:
• Keep patient warm to prevent coagulopathy
• If epistaxis is caused by major trauma, always examine from for other injuries
For those not in extremis, use gold-standard first aid (also known as Trotter’s or Hippocratic method):
• Sit with head forward over a basin/sink
• Pinch the fleshy part of the nose (nares) firmly
• Hold the nose for 20 minutes without peeking
• Suck on some ice or place ice packs on the forehead or nape of neck
• Spit out any blood in the mouth: it is emetogenic
At the same time, get important history:
• Laterality, duration, frequency
• Severity, estimated blood loss
• Any contributing or inciting factors
• Family history or bleeding disorder
• Past medical history
• Current medications
Physical Examination:
• Site of bleeding: anterior or posterior
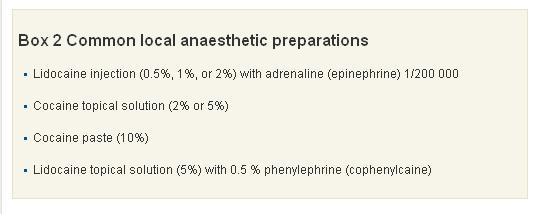
• Suctioning and application of topical local anaesthesia + vasoconstrictors to help with visualisation
• Gently insert Thudicum speculum and spread naris vertically. Use head light for good light source.
• A posterior source of bleeding is suggested by failure to visualise an anterior source, bleeding from both nares, and the visualisation of blood in the posterior pharynx.
Investigations:
• FBC – check haemoglobin level.
• GSH/ GXM
• PT/ INR- Coagulation studies are only of benefit in patients with a known coagulopathy or chronic liver disease, and should not be routine in patients presenting with epistaxis.
• Other bloods test should only be ordered if past medical history warrants further investigation (renal failure = U&E, chronic alcohol abuse = LFTs), and literature has shown they rarely change your management and add considerably to the cost of treating these patients.
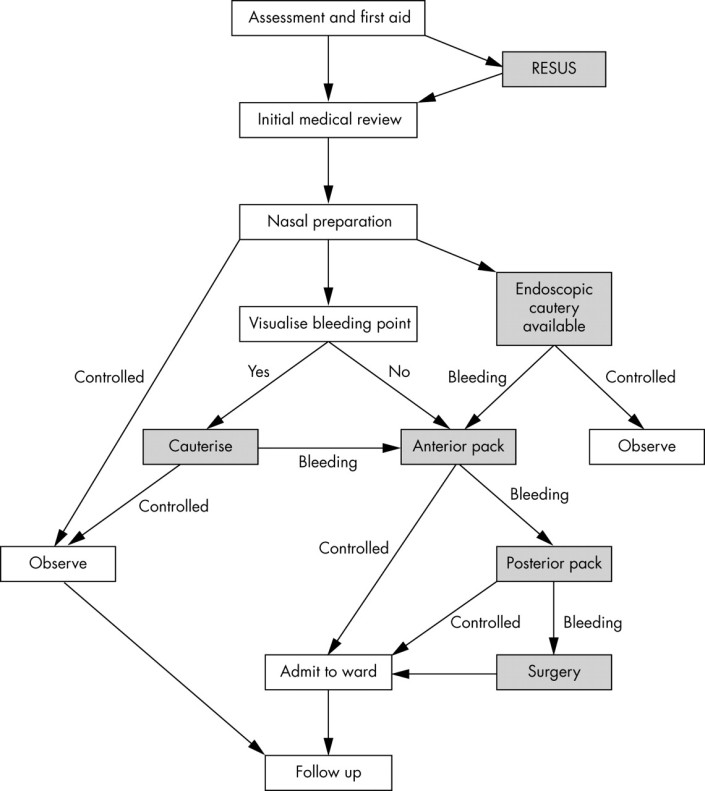
Cautery
1. Silver nitrate stick (75% silver nitrate, 25% potassium nitrate BP w/w): causing chemical damage to mucosal lining
– Careful removal of excess silver nitrate helps prevent staining of the vestibule or upper lip. If staining does occur, it should be neutralised immediately by applying normal saline.
– Only one side of the septum should be cauterised ( risk of septal perforation resulting from decreased vascularisation to the septal cartilage)
– Four to six week interval between cautery treatments to prevent septal perforation
2. Diathermy (Electrocautery)
– an electrical circuit that heats up a metal loop.
– thermal energy seals the bleeding vessel by radiation, not by direct contact
– complication: heat damage to the anterior nares and inferior turbinate.
Anterior packing
The nose should be packed if bleeding continues despite cautery or if no obvious bleeding is seen.
1. Merocel

Correct insertion of a nasal tampon (note that the direction is along the floor of the nasal cavity).
2. Rapid Rhino is an example of a carboxymethylcellulose pack. This is a hydrocolloid material, which acts as a platelet aggregator and also forms a lubricant on contact with water. Unlike Merocel, it has a cuff that is inflated by air and the hydrocolloid or Gel-Knit is supposed to preserve newly formed clot during removal.

3. Ribbon gauze. Pre-prepared packs eg: Vaseline or bismuth-iodoform paraffin paste impregnated packs.
If still bleeding:
Posterior packing
1. Foley catheter – use size 16 for adult
Inserted through the anterior nares and passed back until the tip is seen in the oropharynx. It is then inflated with 3–4 ml of water or air.
The catheter is pulled forward until the balloon engages the posterior choana. The nasal cavity is then packed anteriorly with ribbon gauze or a nasal sponge. The balloon is held firmly in place with an umbilical clamp at the anterior nares.
Protect the columella with a soft dressing, otherwise it is susceptible to pressure necrosis.
Other complications include posterior displacement of the balloon with potential airway compromise, deflation in situ (which is more likely to occur with air inflation) and rupture of the balloon, which when it contains water, could result in aspiration.
2. Brighton balloon
This is specifically manufactured for the treatment of epistaxis. It has a postnasal balloon and a mobile anterior balloon that are independently inflated.
 Sagittal view of the nasal cavity with a Brighton balloon in situ.
Sagittal view of the nasal cavity with a Brighton balloon in situ.

http://bestpractice.bmj.com/best-practice/monograph/421/treatment/step-by-step.html
- ADMIT WARD
- START ANTIBIOTIC – to prevent Toxic Shock Syndrome
- REMOVE PACKING AFTER 48 HOURS
- IF STILL BLEEDING, PACK AGAIN
- BRING PATIENT TO OT FOR EUA, KIV PROCEED
Surgery:
Diathermy
The localisation of a bleeding point under general anaesthetic is easier because of improved nasal access and instrumentation. The use of bipolar rather than monopolar diathermy is recommended, as there are reports of optic or oculomotor nerve damage.
Septal surgery
Septal surgery is sometimes performed to allow access to the nasal cavity. As most haemorrhages occur from the septum, raising a mucoperichondral flap during septal surgery can be beneficial as this will decrease blood flow to the mucosa, which often in itself stems bleeding. Surgery is also used to correct a deviated septum or remove a septal spur, which may be the cause of epistaxis. This occurs either by altering air flow through the nose or in severe cartilage deformities, by persistent mucosal irritation.
Sphenopalatine artery ligation
Anterior/posterior ethmoidal artery ligation
Internal maxillary artery ligation
The approach is a modified Caldwell-Luc operation, through the posterior wall of the maxillary sinus into the pterygopalatine fossa. The maxillary vessel can be either clipped or diathermied. Complications of this include devitalised gums and teeth, sinusitis, and problematic intraoperative bleeding.
External carotid artery ligation
Angiographic embolisation
Complications of nasal packing
• Toxic shock syndrome
• Blockage of
– nasolacrimal duct leading to epiphora
– sinus drainage leading to acute sinusitis
– nasal airway leading to hypoxia
• Nasovagal reflex: this reflex occurs during insertion of a pack or instrumentation of the nasal cavity. It leads to vagal stimulation, with consequent hypotension and bradycardia
• Sleep apnoea, attributable to decreased nasal air entry leading to hypoxia during somnolence
• Displacement of pack into oropharynx with risk of acute airway obstruction
References/ Sources:
1. http://lifeinthefastlane.com/epistaxis/
2. http://pmj.bmj.com/content/81/955/309.full
