Head and Neck
LINGUAL THYROID
Short Notes 2005
Lingual thyroid is caused by a rare developmental disorder due to aberrant embryogenesis during the descent of thyroid gland to the neck.
It is the most frequent ectopic location of thyroid gland.
The incidence of LT is reported as 1:100,000.
It is 7 times higher in females.
Hickmann recorded the first case of lingual thyroid in 1869. Montgomery stressed that for a condition to be branded as lingual thyroid, thyroid follicles should be demonstrated histopathologically in tissues sampled from the lesion
Development:
Early in embryogenesis, thyroid gland appears as proliferation of endodermal tissue in the floor of the pharynx between tuberculum impar and hypobranchial eminence (this area is the later foramen caecum).Normally thyroid gland descends along a path from foramen cecum in the tongue, passes the hyoid bone, to the final position in front and lateral to the second, third, and fourth tracheal rings by 7 weeks gestation. During this descent thyroid tissue retains its communication with foramen cecum. This communication is known as thyroglossal duct. Once the thyroid reaches its final destination, the thyroglossal duct degenerates.
Persistence of thyroglossal duct even after birth leads to the formation of thyroglossal cyst. These cysts usually arise from the remnants of thyroglossal duct and can be found anywhere along the migration site of thyroid gland. This descent may arrest anywhere along this path and this condition may remain unnoticed until puberty. Any functioning thyroid tissue found outside of the normal thyroid location is termed ectopic thyroid tissue. Although it is usually found along the normal path of development, ectopic tissue has also been noted in the mediastinum, heart, esophagus, and diaphragm. Lingual thyroid is the result of failure of descent of the thyroid anlage from the foramen cecum of the tongue. The reasons for the failure of descent are unknown.
Clinical presentations:
Majority of these patients are asymptomatic.
oropharyngeal obstruction may include dysphagia (mild or severe), dyspnea and dysphonia, fullness in the throat, sleep apnoea.
Stridor is most common in neonates.
About 33% of the patients show hypothyroidism findings.
Bleeding is rarely described.
The clinical presentation of LT could be classified into two groups according to the appearance of the symptoms: infants and young children whose lingual thyroid is detected via routine screening may suffer from failure to thrive and mental retardation, or even severe respiratory distress, resulting in a medical emergency. Other cases may present with onset of slowly progressing dysphagia and symptoms of oropharyngeal obstruction before or during puberty. This occurs as a response to the increased demand for thyroid hormone in these hypermetabolic states. Similar response is also encountered during other metabolic stress conditions like pregnancy, infections, trauma, menopause, etc.
head and neck examination :
midline, nodular pinkish mass in the base of the tongue. On palpation this mass could be felt as solid firm and fixed mass. It would be seen attached to the tongue at the junction of anterior 2/3 and posterior 1/3. approximately foramen cecum is supposed to be present. palpate the neck in the region of thyroid to ascertain whether normal thyroid tissue is present in the neck.
Investigations
- thyroid function tests (often demonstrate normal gland functions).
- USG neck no thyroid in neck, Xray neck (globular mass at tongue base hyoid region), CT scan neck
- Technetium scanning confirms the presence of ectopic thyroid tissue at the base of tongue.
- FNAC, LT resembles normal thyroid tissue.
Rx:
1.Suppressive therapy with exogenous thyroid hormone should be tried first in order to decrease the size of the gland.
- surgical removal if emergency. levothyroxine therapy should be initiated after as the lingual thyroid is the only functioning thyroid tissue found in 70% of these patients.
PHARYNGOCUTANEOUS FISTULA
Short Note 2005
-A fistula is an abnormal communication between two epithelialized surfaces.
-Pharyngocutaneous fistula is the most common non-fatal complication following total laryngectomy.
– It creates a communication between the pharynx and cervical skin around the surgical incision or, less frequently, the stoma of the tracheostomy.
– Billroth was also the first person to report PCF as one of the complications of total laryngectomy (he performed first total laryngectomy)
– INCIDENCE reported extremely variable ranging from 3.6% to 65%
CAUSE:
-Total laryngectomy w or w/o pharyngectomy
-Partial laryngectomy
-Commando procedure
PRESENTATION:
-a complication that appears in the early post-operative period after total laryngectomy.
-Usually around 3th to 8th post operative day.
-Pharyngeal contents, usually saliva, flow through the fistula emerging from the cutaneous orifice
– Mean hospitalization time is usually 13 – 15 days in comparison to 3 – 5 days for other patients.
-increased morbidity, delay in adjuvant treatment, prolonged hospitalization, and high treatment costs
-More common in males than females
CONTRIBUTING FACTORS:
- Time of oral feeding Initiating oral feeding within 48 hours of total laryngectomy without partial pharyngectomy; who have not had a previous surgical resection of the upper aerodigestive tract; and who have either not received previous therapeutic irradiation to the head and neck region; does not increase the frequency of PCF. Oral feeding especially with solid food encourages granulation tissue formation along the fistula tract and eventually results in more spontaneous closure of the fistula tract.
- Age – > 60 yrs more predisposed.
- Gastroesophageal reflux disease(GORD) Prophylactic use of ranitidine (H2 receptor blocker) and metoclopramide (prokinetic) has decreased the incidence of pharyngo-cutaneous fistula
- Preoperative tracheostomy contributes to post total laryngectomy PCF fistula formation
- Tumor stage and laryngeal site Glottis Ca > Supraglottis > Pyriform sinus > Subglottis
- Preoperative Hb: Low preoperative Hb increases the incidence of PCF nine-fold
- Preoperative radiation: Related to increase of the radiation field size, dose increment and a change from continuous to fractionated radiation therapy 8. Malnutrition
- Suture material: There is a statistically significant difference in the formation of PCF between vicryl and catgut groups in favor of vicryl which has greater tensile strength, less inflammatory reaction and has a longer half- life Staples have shown a much lesser incidence of PCF
- Positive surgical margins: Presence of infiltrated margins may explain the higher frequency of fistula formation as a result of deficient healing process occurring at the surgical wound, where the presence of the tumor cells may negatively influence the healing process and wound closure. 11. Vascular diseases related to smoking and alcohol drinking
| Early diagnosis is important: Less risky for sepsis and major vessel rupture More conservative and easy management |
| Early sign of impending Pharyngocutaneous fistula: Persistent low-grade fever: 38.5C wound erythema and edema localized tenderness in central neck near the wound wound infection unresponding to conservative treatment saliva seen at wound or in the drain tube esophagogram: sinus tract> 2 cm barium methyl blue swallowing test (+) definitive fistula formation |
|
Conservative management: Residual tumor should be excluded firstly Surgical intervention is reserved when failed by Conservative management Methods: Drainage: Saliva accumulation ->abscess formation ->flap necrosis and sepsis Goal: infection control and prevention of large fistula If suction drain tube (+), delay removal or shift to penrose for drainage If no drain tube: Small: Repeated aspiration Large with abscess formation: open drain: Away from the stoma: prevention of aspiration Temporal pharyngostoma-> secondary reconstruction Silicone septal button with stoma bag (khan 1993) Removal and curettage of necrotic tissue Pressure dressing for flap down Tube feeding with adequate nutrition Infection control: systemic antibiotics: aerobic and anaerobic. Time: small fistula without infection< 2-3 weeks Most: less than 40 days |
| Surgical management:
PCF have been classified according to source of tissue used in reconstruction to three types: The pectoralis major flap offers the benefit of an excellent vascular pedicle. The latissimus dorsi and the trapezius flaps much less advantageous than the versatile, durable pectoralis major. Muscle flaps Sternocleidomastoid muscle flap is also used for fistula closure which has advantages of workable mass, good coverage and single stage reconstruction. |
AMELOBLASTOMA
A.K.A: Adamantinoma of the jaw ( Short Note 2003 )
Definition:
Benign, locally aggressive tumours that arise from the mandible, or less commonly from the maxilla.
Epidemiology:
Ameloblastomas are the second most common odontogenic tumour (odontoma is the most common)
3rd to 5th decades of life
No gender predilection
Clinical presentation:
Hard painless slow growing mass near the angle of the mandible in the in the region of the 3rd molar tooth (48 and 38)
Can occur anywhere along the alveolus of the mandible (80%) and maxilla (20%).
When the maxilla is involved, the tumour is located in the premolar region, and can extend up in the maxillary sinus.
Although benign, it is a locally aggressive neoplasm with a high rate of recurrence. Approximately 20% of cases are associated with dentigerous cysts and unerupted teeth.
Pathology:
Arise from ameloblasts, which are part of the odontogenic epithelium, responsible for enamel production and eventual crown formation.
Three variants are described:
simple (no nodule): best prognosis
luminal: single nodule projecting into the cyst
mural: multiple nodules (often only microscopic) in the wall of the cyst
Radiographic features
Plain film and CT
It is classically seen as a multiloculated (80%), expansile “soap-bubble” lesion, with well demarcated borders and no matrix calcification.
MRI
In general ameloblastomas demonstrate a mixed solid and cystic pattern, with a thick irregular wall, often with papillary solid structures projecting into the lesion.
Treatment and prognosis
surgical en-bloc resection.
Local curettage is associated with a high rate of local recurrence (45-90%).
Simple unicystic lesions are less common but have a better prognosis. Simple (no nodule) variant will not be diagnosable on radiography, as it will be indistinguishable form other more common cysts. Luminal variant, has a single nodule projecting into the cyst.
Mural variant has multiple nodules (often only microscopic) in the wall of the cyst. has an elevated risk of recurrence.
Malignant behaviour is seen in two forms :
- ameloblastic carcinoma
- frankly malignant histology
- malignant ameloblastoma
- metastases despite well differentiated ‘benign’ histology
Differential diagnosis
- dentigerous cyst: the relationship between ameloblastomas and dentigerous cysts is a controversial one, 20% of ameloblastomas thought to arise from pre-existing dentigerous cysts
- odontogenic keratocyst (OKC): usually unilocular with thin poorly enhancing walls
- odontogenic myxoma: can be almost indistiguishable
- aneurysmal bone cyst (ABC)
- fibrous dysplasia
Radiotherapy in Head and Neck Cancer
Complication of radiotherapy:
Early
- Skin – erythema, desquamation
- Mucosa – mucositis, dry mucosa
- Candidiasis
- Loss of appetite, nausea, vomitting ( Radiation sickness )
- Laryngeal edema
- Haematopoietic suppression
Late
- Skin – atrophy, fibrosis of subcutaneous tissue
- Xerostomia
- Eye – retinopathy, cataract
- Teeth – decay, osteoradionecrosis
- Trismus ( fibrosis of TMJ and muscles of mastication)
- Endocrine deficit – thyroid, pituitary
- Transverse myelitis
- Radiation induced malignancy – thyroid cancer, osteosarcoma
Why patients undergoing Radiotherapy need to have Hemoglobin level above 10g/dl?
- Low Hb —> low oxygen carrying capacity —> low oxygen —> less radiation-induced cytotoxic free radicals to kill the tumour cells
- Free radicals formation: O2 ——> O+ + O+
H2O ——> O+ + OH-
Is inappropiately high Hb good for radiotherapy?
- No. Increased blood viscosity —-> reduces tumour cell perfusion —–> less free radicals to kill the tumour cells
RELEVANT ANATOMY OF LARYNX
VAGUS NERVE
Larynx supplied by vagus nerve
The vagus nerve has three nuclei located within the medulla:
1. The nucleus ambiguus – the motor nucleus
2. The dorsal nucleus – innervate the involuntary muscles of the bronchi, esophagus, heart, stomach, small intestine, and part of the large intestine.
3. The nucleus of the tract of solitarius -carry sensory fibers from the pharynx, larynx, and esophagus.
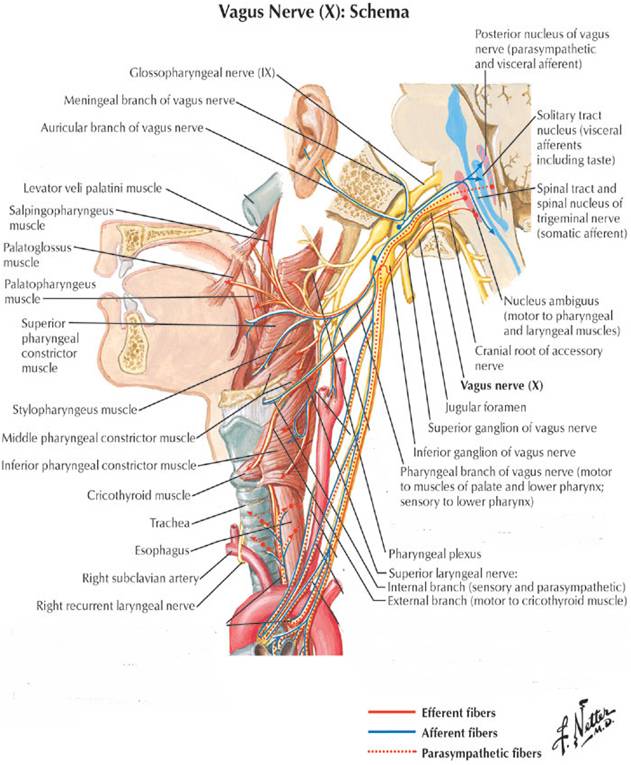
Upper motor neurons from cerebral cortex to nucleus ambiguus in the medulla
Lower motor neurons from nucleus ambiguus exit the medulla as the vagus nerve
Vagus nerve exits the skull base via the jugular foramen
Branches:
Pharyngeal branch
Superior laryngeal nerve
Recurrent laryngeal nerve
Superior laryngeal nerve
1. Internal branch – pierce thyrohyoid membrane to supply sensation of larynx above the VC
2. External branch –at the upper pole of thyroid gland and supply cricothyroid muscle ( the tensor of VC which controls vocal fold lengthening and pitch)
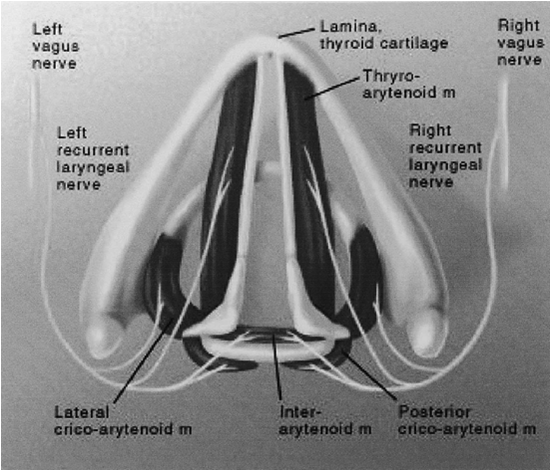
Recurrent laryngeal nerve
• Left – arches around arch of aorta lateral to liagmentum arteriosum, then nters TE groove
• Right –arches around Right subclavian artery, then enter TE groove at 45 degree angle
• Behr’s triangle:
superior: inferior thyroid artery
lateral: common carotid artery
medial: recurrent laryngeal nerve
• Enters the larynx beneath the cricopharyngeal muscle
• Motor supply to all intrinsic muscles of the larynx except cricothyroid and sensory supply to larynx below VC
MUSCLES OF THE LARYNX
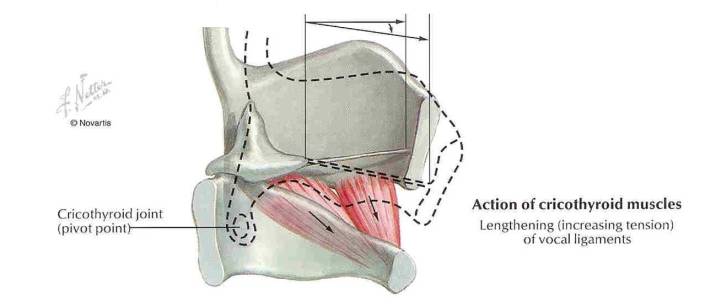
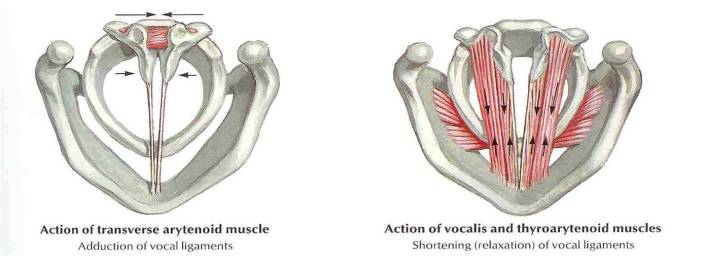
1. Cricothyroid
2. Posterior cricoarythenoid
3. Lateral cricoarythenoid
4. Transverse arythenoid
5. Oblique arythenoid
6. Thyroarythenoid (vocalis)
Tonsillectomy
Blood supply & relation of tonsils:
Tonsillectomy:
Surgical procedure that completely removes the tonsil, including its capsule by dissecting the peritonsillar space between the tonsil capsule and the muscular wall.
Indication for tonsillectomy:
- Recurrent infections of throat: (typically group A betahemolytic streptococcal)
- 7 or more episodes in 1 year
- 5 or more episodes per year in 2 years
- 3 or more episodes per year in 3 years
- 2 weeks or more of lost of school or work in a year
2. Peritonsillar abscess
- Children: 4-6 weeks after the 1st episode
- Adult: after 2nd episode
3. Tonsillitis causing febrile seizure
4. Tonsillar hypertrophy causing airway obstruction (OSA)
5. Suspicion of malignancy eg unilateral tonsillar hypertrophy eg: extranodal intratonsillar lymphoma, SCC tonsil
6. Chronic tonsillitis
Complications:
Early:
- Primary hemorrhage (at time to surgery)
- Reactionary hemorrhage (within 48hours post op) because a clot in a vessel has been displaced, or a ligature has slipped.
- Injury to tonsillar pillars, uvula, soft palate, tongue, teeth
- Aspiration (prevention: throat pack)
- Difficult intubation causing laryngospasm, laryngeal edema
Late:
- Pain
- Secondary hemorrhage – 8 to 14 days later when the wound has become infected and eroded a vessel.
- Infection
- Altered taste (dysgeusia)- due to injury to glossopharyngeal nerve
- Referred otalgia
Unusual complications:
- Necrotizing fasciitis
- Surgical emphysema due to injury to superior contrictor muscle
- Velopharyngeal insufficiency
- Hemotoma at lingual / BOT
- Mediastinitis
- Atlantoaxial subluxation
Intraoperatively if you encounter bleeding, how do you stop the bleeding?
- Tonsillar square with or without adrenaline to give compression and pack the area
- Coagulate or cauterize using bipolar diathermy
- Tie ~ use Burkitt artery forcep and then tie
Management for unilateral tonsil enlargement:
Assess:
- Size
- Appearance
- Neck nodes/ swelling
- Constitutional symptoms
- Pain
- Bleeding
If suspicious of malignancy – do tonsillectomy
If not, give 1 course of antibiotic and reassess.
Causes for unilateral tonsillar enlargement:
Divided into: anatomical variation, infective and neoplasm
Neoplasm
- Lymphoma
- SCC
Infective
- Tuberculosis
- Actinomycosis
- Paratonsillar abscess or peritonsillitis pushing tonsil medially
Anatomical variations
- asymmetrical tonsillar depth or tonsillar pillars
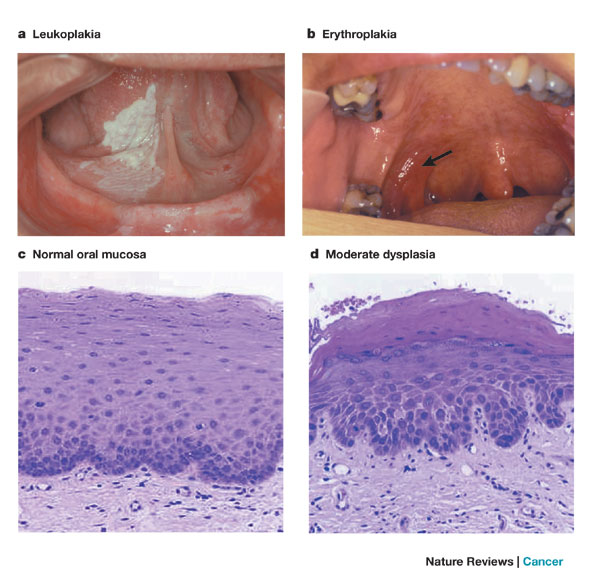
Leukoplakia
Definition of Leukoplakia:
- Premalignant condition
- Characterised by a white patch or plaque that cannot be characterized clinically or histologically as any other disease. (WHO Definition)
How does Verrucous Carcinoma differ from SCC?
Verrucous Carcinoma: “Ackerman’s tumor.” – 1st described by Ackerman
- Uncommon variant of SCC, locally aggressive, clinically exophytic, low-grade, slow-growing, well-differentiated squamous cell carcinoma with minimal metastatic potential.
- Risk factors: tobacco chewing, oral snuff “Snuff dipper’s cancer”, smoking, alcohol, betel nut chewing
- Good prognosis. Local recurrence is not uncommon, but metastasis to distant parts of the body is rare.
- Painless, thick white plaque resembling a cauliflower (warty lesion)
- Commonest site: Oral cavity
- Treatment: Wide local excision or radiotherapy