Larynx
Cordectomy
Cordectomy classification:
- Subepithelial cordectomy – resection of epithelium ( Type I)
- Subligamental cordectomy – resection of Reinke’s space and vocal ligament ( Type II )
- Transmuscular cordectomy – through vocalis muscle ( Type III )
- Total cordectomy ( Type IV )
- Extended cordectomy (Type V)
Va – encompasses anterior commissure and contralateral vocal folds
Vb – includes arythenoids
Vc – includes subglottis
Vd – includes ventricle
VOCAL CORD PALSY / IMMOBILITY
VOCAL CORD PALSY / IMMOBILITY
Bilateral vocal fold (vocal cord) immobility (BVFI) is a broad term that refers to all forms of reduced or absent movement of the vocal folds.
Bilateral vocal fold (cord) paralysis (BVFP) refers to the neurologic causes of bilateral vocal fold immobility (BVFI) and specifically refers to the reduced or absent function of the vagus nerve or its distal branch, the recurrent laryngeal nerve (RLN).
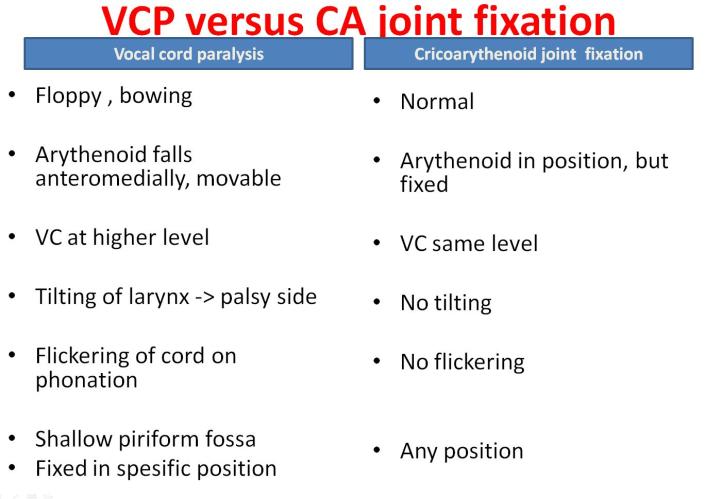
Vocal fold immobility may also result from mechanical derangement of the laryngeal structures, such as the cricoarytenoid (CA) joint.
What Are the Symptoms?
Both paresis and paralysis of voice box muscles result in:
Voice changes: Hoarseness; breathy voice; extra effort on speaking; excessive air pressure required to produce usual conversational voice; and diplophonia (voice sounds like a gargle).
Assess GRABAS score:
G rade (overall) of hoarseness
R ough
B reathy
A sthenic (weakness or lack of power in voice)
S trained
0=normal 1=slight 2=Moderate 3=Extreme
Airway problems: Shortness of breath with exertion, noisy breathing, and ineffective cough.
Swallowing problems: Aspiration symptoms – choking or coughing when swallowing food or drink. Cough with fever.
Also ask about reflux.
Classification
Laterality:
1. Unilateral vocal cord paralysis is most common.
2. Bilateral
Complete/ Incomplete
Incomplete paralysis
1. RLN palsy
Left (75%) , Right (15%) , BL (10%)
Abductor, adductor
2. Superior laryngeal nerve palsy
Cricothyroid muscles
Combine / complete paralysis
Causes
Systemic
Idiopathic
Localized caused
Supranuclear
Nuclear : nucleus ambigius
High vagal : combined lesion
Low vagal : RLN palsy
Central neurologic abnormalities
Causes bilateral vocal fold paralysis (BVFP)
Eg:
1. Arnold-Chiari deformity with meningomyelocele – the most common abnormality.
2. Other CNS insults (eg, infarct, craniotomy, asphyxia)
Aetiology: M2ATI3N
Malignant : (30% cases)
o Lung carcinoma 50%
o Esophageal carcinoma 20%
o Thyroid 10%
Iatrogenic:
o Thyroidectomy
o Esophagectomy
o Pneumonectomy
o CABG
Trauma:
o Penetrating neck or chest trauma.
o Post intubation
o Whiplash injuries
Neurological (5-10%)
o Poliomyelitis
o Multiple Sclerosis
o Myasthenia Gravis
o Guillian-Barre
o Wallenberg syndrome (lateral medullary stroke)
o Syringomyelia
o Encephalitis
o Parkinsons
o Diabetes Mellitus
o Ortner’s syndrome (left atrial hypertrophy)
Autoimmune:
o Rheumatoid arthritis – “fixed” cord
o Sarcoidosis
o Lupus
o Polyarteritis nodosa
Infectious:
o Syphilis
o Tuberculosis
o Thyroiditis
Idiopathic (20-25%): Viral causes ( viral neuritis usually on Right VC)
Medications
Vinca alkaloids – in children ungoing chemotherapy for lymphoma
o Vincristine and vinblastine
o Unilateral or bilateral
o Dose related
o Resolves with dose adjustment or cessation
SEMON’S LAW
Rosenbach(1880) & Semon (1881)
In all progressive organic lesions, abductor fibres of recurrent laryngeal nerve are more susceptible and thus first to be paralyzed compared to adductor fibres
• WHY ?
1. Nerve fibres supplying abductors are in periphery of RLN
2. Muscle bulk for the abductors is less, more susceptible
3. Phylogenetically, larynx main function is protection, so adductor function are maintained
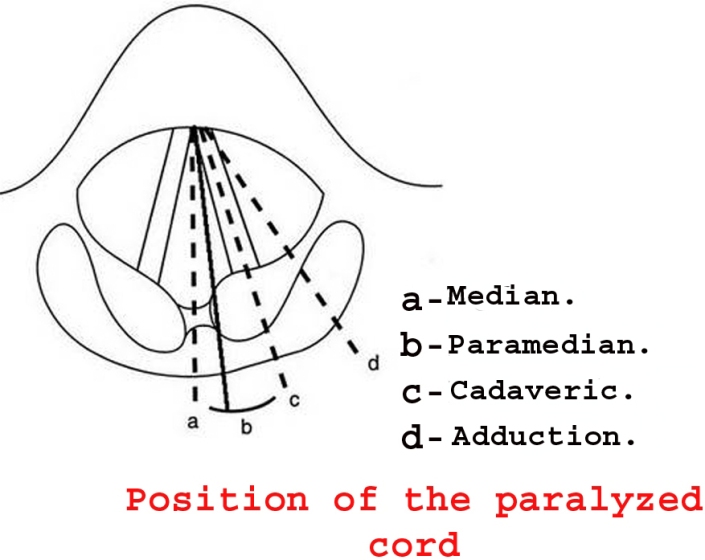
In progressive vocal cord palsy, vocal cord position will be in median or paramedian first, then later when the adductor fibres are also paralyzed, the vocal cord will be in cadaveric position.
Wegner and Grossman Theory : <popular theory>
• “In the absence of cricoarytenoid joint fixation, an immobile vocal cord in paramedian position has total pure unilateral recurrent nerve paralysis, and an immobile vocal cord in lateral position has a combined paralysis of superior and recurrent nerves (the adductive action of cricothyroid muscle is lost)”
• RLN palsy (intact SLN) – vocal cord in paramedian position (because cricoarythenoid adducts)
• RLN and SLN palsy – vocal cord in cadaveric position
Final position of paralysed VC is not static & determined by :
1. Vocal fold
– Length of VC
– Mass of VC
– Contour of VC
2. Muscle
– Atrophy
– Fibrosis
3. Nerve
– Synkinesis ( mass movement of all intrinsic muscles due to misinnervation)
– Reinnervation
4. Joint
– Ankylose
RELEVANT ANATOMY OF LARYNX
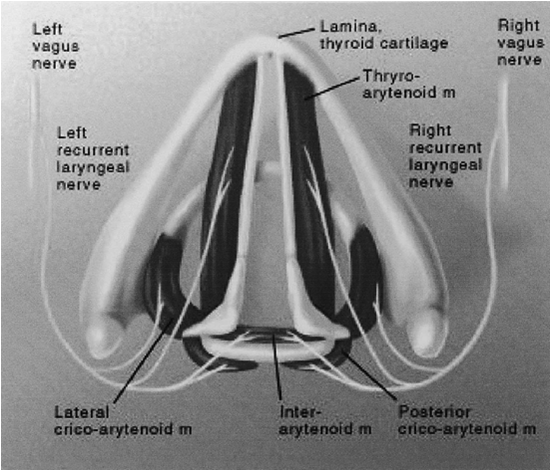
VAGUS NERVE
Larynx supplied by vagus nerve
The vagus nerve has three nuclei located within the medulla:
1. The nucleus ambiguus – the motor nucleus
2. The dorsal nucleus – innervate the involuntary muscles of the bronchi, esophagus, heart, stomach, small intestine, and part of the large intestine.
3. The nucleus of the tract of solitarius -carry sensory fibers from the pharynx, larynx, and esophagus.
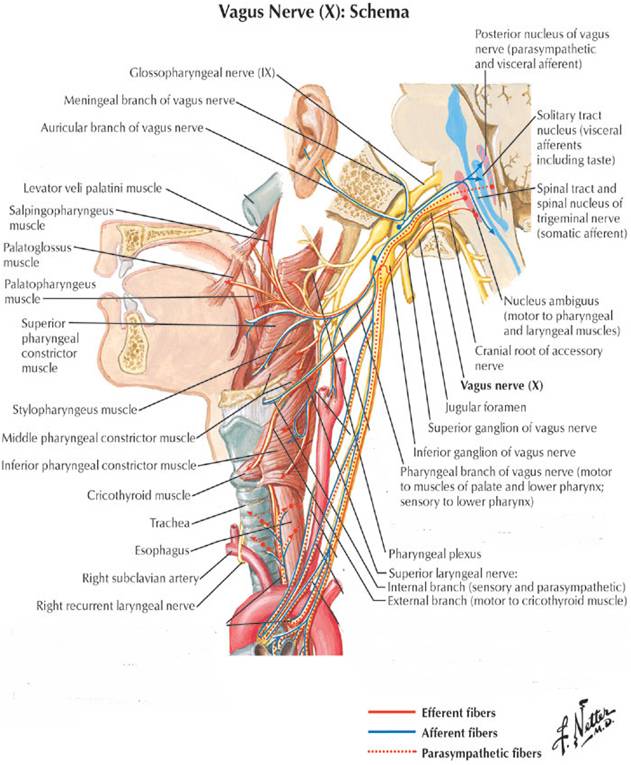
Upper motor neurons from cerebral cortex to nucleus ambiguus in the medulla
Lower motor neurons from nucleus ambiguus exit the medulla as the vagus nerve
Vagus nerve exits the skull base via the jugular foramen
Branches:
Pharyngeal branch
Superior laryngeal nerve
Recurrent laryngeal nerve
Superior laryngeal nerve
1. Internal branch – pierce thyrohyoid membrane to supply sensation of larynx above the VC
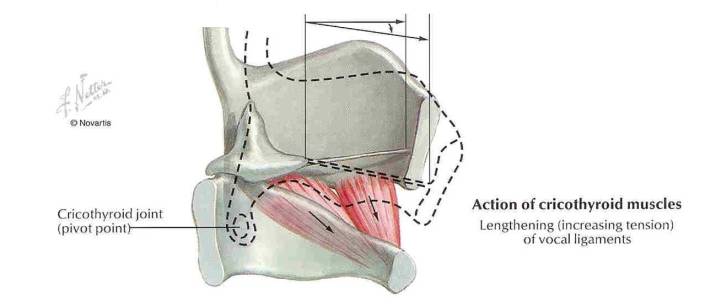
2. External branch –at the upper pole of thyroid gland and supply cricothyroid muscle ( the tensor of VC which controls vocal fold lengthening and pitch)
Recurrent laryngeal nerve
• Left – arches around arch of aorta lateral to liagmentum arteriosum, then nters TE groove
• Right –arches around Right subclavian artery, then enter TE groove at 45 degree angle
• Behr’s triangle:
superior: inferior thyroid artery
lateral: common carotid artery
medial: recurrent laryngeal nerve
• Enters the larynx beneath the cricopharyngeal muscle
• Motor supply to all intrinsic muscles of the larynx except cricothyroid and sensory supply to larynx below VC
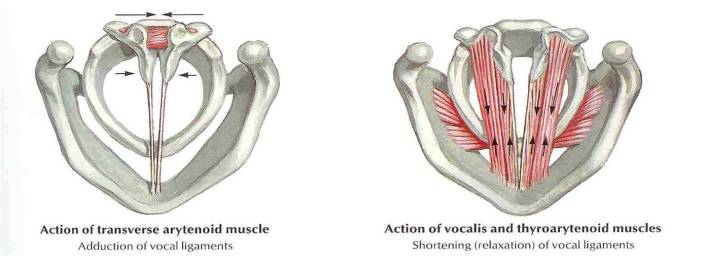
MUSCLES OF THE LARYNX
1. Cricothyroid
2. Posterior cricoarythenoid
3. Lateral cricoarythenoid
4. Transverse arythenoid
5. Oblique arythenoid
6. Thyroarythenoid (vocalis)
Stroboscopy
What is videostroboscopy?
It is a method used for viewing and recording the vocal cord vibration and mucosal wave whereby digital computer and strobe light are used to make the images of the vocal cord vibrations appear in slow motion, so that any abnormal patterns of vibration may be detected.
What are the advantages of videostroboscopy?
- The vibrations of the vocal cords are much too rapid to be observed by the unaided eye under a regular light source. Stroboscopy provides illumination of the larynx with quick pulses of light, which allows for detailed assessment of vocal cord movement in terms of vocal cord movement
- Helps the speech pathologist, physician and patient to obtain a better understanding of the way the vocal folds are functioning, and develop a specific treatment plan.
- The information acquired from the stroboscopic examination of the vocal folds is essential for planning effective phonomicrosurgery (endoscopic surgery to enhance vocal function).
- Structural or tissue abnormalities may be detected as well.
- If a repeat videostroboscopy is needed at a later date, the results can be compared to the previous exam. This allows the voice care team to evaluate the patient’s progress.
- Formal reports, still photos and portions of the video examination can be provided to the patient.
Procedure:
The procedure itself lasts for just 10-15 minutes. A rigid telescope is placed into the mouth OR a small flexible telescope is placed into the nose. The scope will be in the mouth or nose for just a brief time (no longer than 1 minute at a time, usually), and you will always be able to breathe during the test. You will be asked to say various sounds, and a video of the vocal cords will be displayed on a television monitor. (The recording will be replayed later)
Sedation:
A light spray of topical anesthetic may be used if needed, but there is no sedation necessary. The anesthetic is sweet-tasting, and usually wears off in about 15-20 minutes. There is no need to arrange for someone to drive you to and from the appointment.
(Referance: http://www.ent-stl.com/)
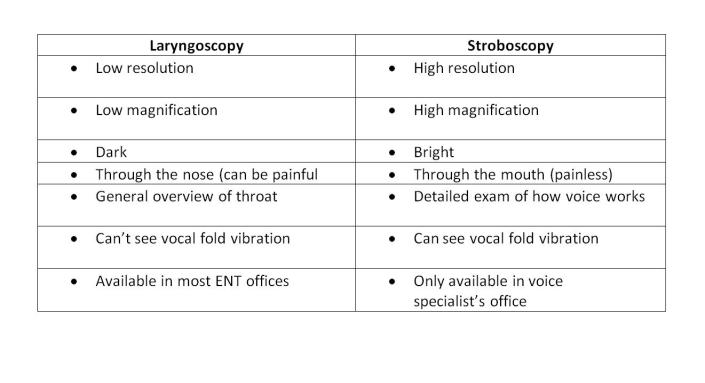
What is the difference between laryngoscopy and stroboscopy?
Info from: http://www.ohniww.org/
It it is critical in cases of voice problems to have a stroboscopy to accurately diagnose and treat your voice problem.
Links for video stroboscopy:
https://www.youtube.com/watch?v=mJedwz_r2Pc
Laryngeal surgery
Classification of laryngeal surgery:
Divided into endoscopic and open techniques. Open techniques divided into expansion and resection.
- Endoscopic:
- Dilatation – bougie, balloon
- LASER: shapshay
- Cold instrumentation
- Open:
Expansion:
- LTR
- Anterior split
- Posterior split
- Antero posterior split
Put costal cartilage graft for expansion or tracheal mucosal flap
Resection:
- Cricotracheal resection (CTR)
- Tracheal resection and anastomoses (TRA)
- Cricotracheal resection and anastomoses (CTRA)
T tube
Why T tube is better than Shilley tube?
- Self cleansing
- Stent the upper limb of segment
Immediate Complications of Post Operative TRA
- Anastomotic leak —> subcutaneous emphysema
- Hematoma
- Pneumon
- Local infection – SSI, hemorrhage
- DVT
Other complications:
- Recurrent stenosis
- Laryngeal dysfunction causing VC palsy (50% temporary)
Contraindications of TRA:
- Less than 1cm from VC (in children between 3mm to 5mm)
- Length of stenosis >4cm (must have adequate trachea for anastomoses)
- Tracheomalacia
- Multilevel stenosis
- Previous RT
- Failed larynhotracheal reconstruction before
- Poor pulmonary function – assess single breath counting, PEFR, FEV1
- Debilitating medical illnesses- COAD, uncontrolled DM
- Vocal cord immobility
Prognosis of surgery depends on:
- Age
- Comorbid
- Site of stenosis: Subglottic stenosis, trachea stenosis
- Grade of obstruction – CM grading
- Length of stenosis
- Tracheomalacia
- Presence of tracheostomy at time to resection
- Presence of 2′ airway pathology
- VC – normal mobility or impaired
- Obese, thick neck, neck circumference —> increase complications
Stenting in larynx:
- Stable larynx ie: expansion with anterior graft doesn’t need stent
- Unstable larynx ie: expansion with anteroposterior graft needs stent
- Stent causes granulation tissue so must aim to take out by 6 weeks
- Types of stents: Rubber stent, LTMOLD stent
Bougie vs Balloon dilatation:
Bougie:
- Free , not costly
- Shearing force –> increase reformation of stenosis due to scarring ( not good)
Balloon: RM1k ++
- Expensive
- Radial force –> less epithelial injury, less scar contraction (good)
Leukoplakia
Definition of Leukoplakia:
- Premalignant condition
- Characterised by a white patch or plaque that cannot be characterized clinically or histologically as any other disease. (WHO Definition)
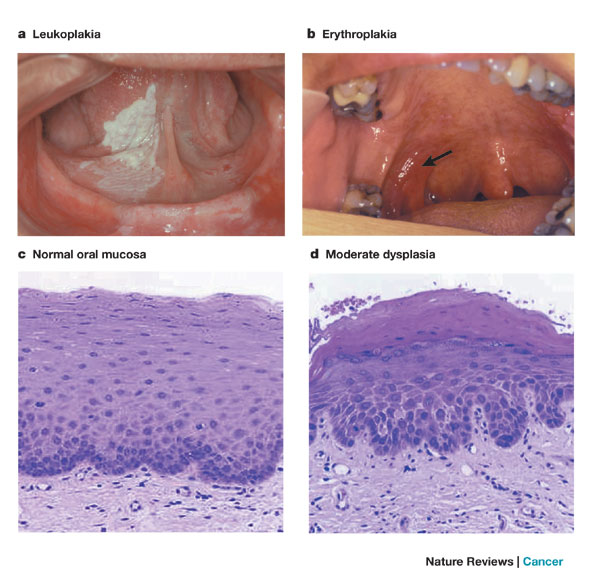
How does Verrucous Carcinoma differ from SCC?
Verrucous Carcinoma: “Ackerman’s tumor.” – 1st described by Ackerman
- Uncommon variant of SCC, locally aggressive, clinically exophytic, low-grade, slow-growing, well-differentiated squamous cell carcinoma with minimal metastatic potential.
- Risk factors: tobacco chewing, oral snuff “Snuff dipper’s cancer”, smoking, alcohol, betel nut chewing
- Good prognosis. Local recurrence is not uncommon, but metastasis to distant parts of the body is rare.
- Painless, thick white plaque resembling a cauliflower (warty lesion)
- Commonest site: Oral cavity
- Treatment: Wide local excision or radiotherapy
The 2nd Asia Pasific Paediatric Airway Course & Workshop

I’m attending The Second Asia Pasific Paediatric Airway Course & Workshop in Taipei, Taiwan.
This is a 2-day lectures and workshop, which covers common and important aspects of paediatric airway disease that are relevant to surgical as well as medical disciplines.
A special emphasis on various aspects of paediatric bronchoscopic procedures and techniques are demonstrated.
Hands-on bronchoscopic techniques are augmented on dogs and live surgery demonstrated on paediatric patients.