LINGUAL THYROID
Short Notes 2005
Lingual thyroid is caused by a rare developmental disorder due to aberrant embryogenesis during the descent of thyroid gland to the neck.
It is the most frequent ectopic location of thyroid gland.
The incidence of LT is reported as 1:100,000.
It is 7 times higher in females.
Hickmann recorded the first case of lingual thyroid in 1869. Montgomery stressed that for a condition to be branded as lingual thyroid, thyroid follicles should be demonstrated histopathologically in tissues sampled from the lesion
Development:
Early in embryogenesis, thyroid gland appears as proliferation of endodermal tissue in the floor of the pharynx between tuberculum impar and hypobranchial eminence (this area is the later foramen caecum).Normally thyroid gland descends along a path from foramen cecum in the tongue, passes the hyoid bone, to the final position in front and lateral to the second, third, and fourth tracheal rings by 7 weeks gestation. During this descent thyroid tissue retains its communication with foramen cecum. This communication is known as thyroglossal duct. Once the thyroid reaches its final destination, the thyroglossal duct degenerates.
Persistence of thyroglossal duct even after birth leads to the formation of thyroglossal cyst. These cysts usually arise from the remnants of thyroglossal duct and can be found anywhere along the migration site of thyroid gland. This descent may arrest anywhere along this path and this condition may remain unnoticed until puberty. Any functioning thyroid tissue found outside of the normal thyroid location is termed ectopic thyroid tissue. Although it is usually found along the normal path of development, ectopic tissue has also been noted in the mediastinum, heart, esophagus, and diaphragm. Lingual thyroid is the result of failure of descent of the thyroid anlage from the foramen cecum of the tongue. The reasons for the failure of descent are unknown.
Clinical presentations:
Majority of these patients are asymptomatic.
oropharyngeal obstruction may include dysphagia (mild or severe), dyspnea and dysphonia, fullness in the throat, sleep apnoea.
Stridor is most common in neonates.
About 33% of the patients show hypothyroidism findings.
Bleeding is rarely described.
The clinical presentation of LT could be classified into two groups according to the appearance of the symptoms: infants and young children whose lingual thyroid is detected via routine screening may suffer from failure to thrive and mental retardation, or even severe respiratory distress, resulting in a medical emergency. Other cases may present with onset of slowly progressing dysphagia and symptoms of oropharyngeal obstruction before or during puberty. This occurs as a response to the increased demand for thyroid hormone in these hypermetabolic states. Similar response is also encountered during other metabolic stress conditions like pregnancy, infections, trauma, menopause, etc.
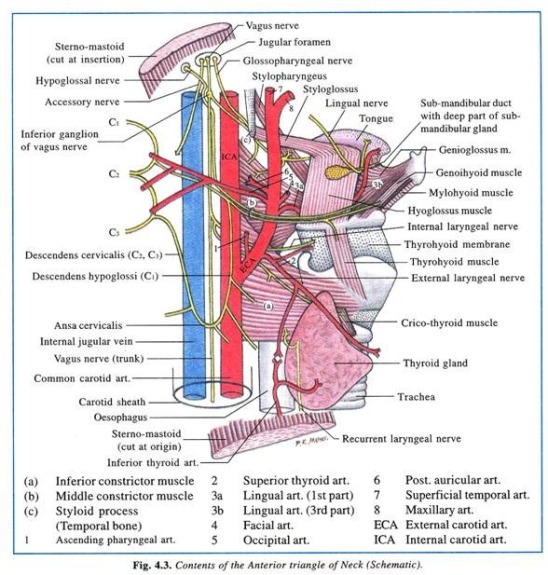
head and neck examination :
midline, nodular pinkish mass in the base of the tongue. On palpation this mass could be felt as solid firm and fixed mass. It would be seen attached to the tongue at the junction of anterior 2/3 and posterior 1/3. approximately foramen cecum is supposed to be present. palpate the neck in the region of thyroid to ascertain whether normal thyroid tissue is present in the neck.
Investigations
- thyroid function tests (often demonstrate normal gland functions).
- USG neck no thyroid in neck, Xray neck (globular mass at tongue base hyoid region), CT scan neck
- Technetium scanning confirms the presence of ectopic thyroid tissue at the base of tongue.
- FNAC, LT resembles normal thyroid tissue.
Rx:
1.Suppressive therapy with exogenous thyroid hormone should be tried first in order to decrease the size of the gland.
- surgical removal if emergency. levothyroxine therapy should be initiated after as the lingual thyroid is the only functioning thyroid tissue found in 70% of these patients.
PHARYNGOCUTANEOUS FISTULA
Short Note 2005
-A fistula is an abnormal communication between two epithelialized surfaces.
-Pharyngocutaneous fistula is the most common non-fatal complication following total laryngectomy.
– It creates a communication between the pharynx and cervical skin around the surgical incision or, less frequently, the stoma of the tracheostomy.
– Billroth was also the first person to report PCF as one of the complications of total laryngectomy (he performed first total laryngectomy)
– INCIDENCE reported extremely variable ranging from 3.6% to 65%
CAUSE:
-Total laryngectomy w or w/o pharyngectomy
-Partial laryngectomy
-Commando procedure
PRESENTATION:
-a complication that appears in the early post-operative period after total laryngectomy.
-Usually around 3th to 8th post operative day.
-Pharyngeal contents, usually saliva, flow through the fistula emerging from the cutaneous orifice
– Mean hospitalization time is usually 13 – 15 days in comparison to 3 – 5 days for other patients.
-increased morbidity, delay in adjuvant treatment, prolonged hospitalization, and high treatment costs
-More common in males than females
CONTRIBUTING FACTORS:
- Time of oral feeding Initiating oral feeding within 48 hours of total laryngectomy without partial pharyngectomy; who have not had a previous surgical resection of the upper aerodigestive tract; and who have either not received previous therapeutic irradiation to the head and neck region; does not increase the frequency of PCF. Oral feeding especially with solid food encourages granulation tissue formation along the fistula tract and eventually results in more spontaneous closure of the fistula tract.
- Age – > 60 yrs more predisposed.
- Gastroesophageal reflux disease(GORD) Prophylactic use of ranitidine (H2 receptor blocker) and metoclopramide (prokinetic) has decreased the incidence of pharyngo-cutaneous fistula
- Preoperative tracheostomy contributes to post total laryngectomy PCF fistula formation
- Tumor stage and laryngeal site Glottis Ca > Supraglottis > Pyriform sinus > Subglottis
- Preoperative Hb: Low preoperative Hb increases the incidence of PCF nine-fold
- Preoperative radiation: Related to increase of the radiation field size, dose increment and a change from continuous to fractionated radiation therapy 8. Malnutrition
- Suture material: There is a statistically significant difference in the formation of PCF between vicryl and catgut groups in favor of vicryl which has greater tensile strength, less inflammatory reaction and has a longer half- life Staples have shown a much lesser incidence of PCF
- Positive surgical margins: Presence of infiltrated margins may explain the higher frequency of fistula formation as a result of deficient healing process occurring at the surgical wound, where the presence of the tumor cells may negatively influence the healing process and wound closure. 11. Vascular diseases related to smoking and alcohol drinking
| Early diagnosis is important: Less risky for sepsis and major vessel rupture More conservative and easy management |
| Early sign of impending Pharyngocutaneous fistula: Persistent low-grade fever: 38.5C wound erythema and edema localized tenderness in central neck near the wound wound infection unresponding to conservative treatment saliva seen at wound or in the drain tube esophagogram: sinus tract> 2 cm barium methyl blue swallowing test (+) definitive fistula formation |
|
Conservative management: Residual tumor should be excluded firstly Surgical intervention is reserved when failed by Conservative management Methods: Drainage: Saliva accumulation ->abscess formation ->flap necrosis and sepsis Goal: infection control and prevention of large fistula If suction drain tube (+), delay removal or shift to penrose for drainage If no drain tube: Small: Repeated aspiration Large with abscess formation: open drain: Away from the stoma: prevention of aspiration Temporal pharyngostoma-> secondary reconstruction Silicone septal button with stoma bag (khan 1993) Removal and curettage of necrotic tissue Pressure dressing for flap down Tube feeding with adequate nutrition Infection control: systemic antibiotics: aerobic and anaerobic. Time: small fistula without infection< 2-3 weeks Most: less than 40 days |
| Surgical management:
PCF have been classified according to source of tissue used in reconstruction to three types: The pectoralis major flap offers the benefit of an excellent vascular pedicle. The latissimus dorsi and the trapezius flaps much less advantageous than the versatile, durable pectoralis major. Muscle flaps Sternocleidomastoid muscle flap is also used for fistula closure which has advantages of workable mass, good coverage and single stage reconstruction. |
ENDOSCOPIC DACRYOCYSTORHINOSTOMY (EDCR)
Short Note 2003
Dacryocystorhinostomy:
Procedure whereby fistula of the lacrimal sac into the nasal cavity is created.
The operative approach to the sac may be external or endoscopic. The latter approach may use rigid telescopes or the microscope.
History:
Endonasal approach to correct nasolacrimal obstruction was described way back in 1800 by Caldwell, West and later during the begining of 1900 by Mosher.
McDonogh was the first to perform endoscopic dacryocystorhinostomy in 1989.
Indications:
- Socially unacceptable epiphora caused by anatomic or functional lacrimal sac or nasolacrimal duct obstruction
- Chronic dacryocystitis with purulent drainage from the canaliculi
- Inflammation of the skin overlying the lacrimal sac in the region of the medial canthus
- Dacryolith formation
- Benign lacrimal sac mass
Advantages of endoscopic DCR:
- better aesthetic result , no external scar.
- any concomittant intranasal pathology causing epiphora can be addressed
- avoids injury to the medial canthus and/or pathologic scar formation.
- preserves the pumping mechanism of the orbicularis oculi muscle.
- active infection of the lacrimal system is not a contraindication to surgery.
- It is especially superior to the external approach in revision surgery.
- less bloody than the external approach.
- the perioperative time is shorter.
- success rate is comparable to the external approach.
Disadvantages of endoscopic DCR:
- It requires specialized training in nasal endoscopic surgery.
- The endoscopic equipment is an expense.
Contraindications of endoscopic DCR:
– Presence of a firm indurated mass above the level
of medial canthus.
– Bloody epiphora
– Presence of bony destruction as seen in
radiological films
– Pseudoepiphora: is essentially reflux tearing: the
main gland over compensates secretion because
of lack of secretion from minor glands of along the
lid margin.
Surgery technique:
– Patient under GA
– Nasal packing with decongestants
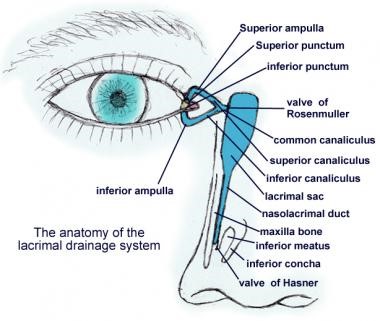
– Localisation of lacrimal sac: the anterior portion of middle turbinate, the sac lies just lateral to it. The lacrimal fossa is bounded by the anterior lacrimal crest, which consists of the frontal process of the maxillary bone. The posterior lacrimal crest is made up of the lacrimal bone itself.
– Mucosal incision: lateral wall mucosa is incised with a sickle knife and is elevated using a Freer elevator. The incision is made vertically from inferior to superior. After elevation the mucosa is removed using a Blakesley forceps.
– Bone removal: To expose the lacrimal sac, the bony lacrimal fossa must be uncovered first. Bone removal can be performed using a Kerrison’s punch forceps or by using a burr.
– Opening of lacrimal sac: After overlying bone removal the lacrimal sac can be incised using a sickle knife. An assistant could tent out the medial wall of the sac with lacrimal probes introduced through the canaliculi. The whole of the medial wall of the sac is removed.
– Topical mitomycin can be applied to the site of surgery to prevent restenosis of the sac.
JONES DYE TESTS
PRIMARY AND SECONDARY
Procedure
- Instil one drop of fluorescein into the conjunctival sac
- Put a cotton bud soaked in anaesthetic in the inferior meatus.
- If fluorescein is detected after five minutes, the system is patent (positive Primary Jones Test)
- If no fluorescein is discovered, this is a negative Primary Jones Test and the functional obstruction could be anywhere from the punctum to the Valve of Hasner.
- Next, wash the excess fluorescein from the conjunctival sac and syringe. If fluorescein is detected, then this shows it had entered the sac and constitutes a positive Secondary Jones Test and suggests a functional obstruction of the nasolacrimal duct.
- If no dye is found on the cotton bud after syringing, this is termed a negative Secondary Jones Test, because fluorescein had not entered the sac and, thus, there is stenosis of the puncta or canalicular system.
- If no saline appears in the nose, there is a complete obstruction somewhere in the lacrimal drainage system.
Hard stop
If the cannula touches the medial wall of the lacrimal sac and lacrimal bone, a definite end point is reached. It indicates that there is no complete obstruction in the canalicular system
Soft stop
If a spongy end point is felt, this indicates that the cannula has been prevented from entering the lacrimal sac. Therefore, there is a blockage in the canalicular system and there will be no distension of the lacrimal sac when the plunger is pressed.
AMELOBLASTOMA
A.K.A: Adamantinoma of the jaw ( Short Note 2003 )
Definition:
Benign, locally aggressive tumours that arise from the mandible, or less commonly from the maxilla.
Epidemiology:
Ameloblastomas are the second most common odontogenic tumour (odontoma is the most common)
3rd to 5th decades of life
No gender predilection
Clinical presentation:
Hard painless slow growing mass near the angle of the mandible in the in the region of the 3rd molar tooth (48 and 38)
Can occur anywhere along the alveolus of the mandible (80%) and maxilla (20%).
When the maxilla is involved, the tumour is located in the premolar region, and can extend up in the maxillary sinus.
Although benign, it is a locally aggressive neoplasm with a high rate of recurrence. Approximately 20% of cases are associated with dentigerous cysts and unerupted teeth.
Pathology:
Arise from ameloblasts, which are part of the odontogenic epithelium, responsible for enamel production and eventual crown formation.
Three variants are described:
simple (no nodule): best prognosis
luminal: single nodule projecting into the cyst
mural: multiple nodules (often only microscopic) in the wall of the cyst
Radiographic features
Plain film and CT
It is classically seen as a multiloculated (80%), expansile “soap-bubble” lesion, with well demarcated borders and no matrix calcification.
MRI
In general ameloblastomas demonstrate a mixed solid and cystic pattern, with a thick irregular wall, often with papillary solid structures projecting into the lesion.
Treatment and prognosis
surgical en-bloc resection.
Local curettage is associated with a high rate of local recurrence (45-90%).
Simple unicystic lesions are less common but have a better prognosis. Simple (no nodule) variant will not be diagnosable on radiography, as it will be indistinguishable form other more common cysts. Luminal variant, has a single nodule projecting into the cyst.
Mural variant has multiple nodules (often only microscopic) in the wall of the cyst. has an elevated risk of recurrence.
Malignant behaviour is seen in two forms :
- ameloblastic carcinoma
- frankly malignant histology
- malignant ameloblastoma
- metastases despite well differentiated ‘benign’ histology
Differential diagnosis
- dentigerous cyst: the relationship between ameloblastomas and dentigerous cysts is a controversial one, 20% of ameloblastomas thought to arise from pre-existing dentigerous cysts
- odontogenic keratocyst (OKC): usually unilocular with thin poorly enhancing walls
- odontogenic myxoma: can be almost indistiguishable
- aneurysmal bone cyst (ABC)
- fibrous dysplasia
CAVERNOUS SINUS THROMBOSIS
Short Note 2003
DEFINITION:
- Formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains deoxygenated blood from the brain back to the heart.
ETIOLOGY:
Usually from a spreading infection in the nose, sinuses, ears, or teeth.
Nasal furuncle (50%), sphenoidal or ethmoidal sinuses (30%) and dental infections (10%).
Less common primary sites of infection include tonsils, soft palate, middle ear, or orbit (orbital cellulitis).
The highly anastomotic venous system of the paranasal sinuses allows retrograde spread of infection to the cavernous sinus via the superior and inferior ophthalmic veins (valveless veins).
Causative organism: Staphylococcus infectious 70% of the cases. Streptococcus is the second leading cause. Gram-negative rods and anaerobes, rarely Aspergillus fumigatus and mucormycosis.
CLINICAL FEATURES:
-abrupt onset of unilateral periorbital edema, headache,
photophobia and proptosis
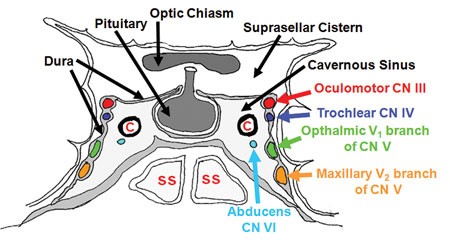
– Ptosis, chemosis, cranial nerve palsies (III, IV, V,VI).
Sixth nerve palsy is the most common. ( it is the content of cavernous sinus while others are located at lateral wall)
– Sensory deficits of the ophthalmic and maxillary branch of the fifth nerve are common.
– Periorbital sensory loss and impaired corneal reflex
– Papilledema, retinal hemorrhages, and decreased visual acuity and blindness may occur from venous – congestion within the retina.
– Fever, tachycardia and sepsis may be present.
– Headache with nuchal rigidity may occur.
– Pupil may be dilated and sluggishly reactive.
– Infection can spread to contralateral cavernous sinus within 24–48 hours of initial presentation.
INVESTIGATIONS:
FBC, ESR, blood cultures, and sinus cultures
Lumbar puncture TRO meningitis.
CT BRAIN/ PNS: Opacification, sclerosis, and air-fluid levels, thickening of the superior ophthalmic vein, and irregular filling defects within the cavernous sinus.
MRI, MR venogram : more sensitive than a CT scan & imaging studies of choice. Findings may include deformity of the internal carotid artery within the cavernous sinus, and an obvious signal hyperintensity within thrombosed vascular sinuses on all pulse sequences.
TREATMENT:
Medical:
- IV Antibiotics: IV Rocephine 2g OD
+/- IV Metronidazole 500mg TDS
- Anticoagulation with heparin is controversial.
- Steroid therapy is also controversial.
Surgical drainage with sphenoidotomy is indicated if the primary site of infection is thought to be the sphenoidal sinuses.
All patients with CST are usually treated with prolonged courses (3–4 weeks) of IV antibiotics. If there is evidence of complications such as intracranial suppuration, 6–8 weeks of total therapy may be warranted.
NECROTIZING OTITIS EXTERNA
1.NECROTIZING OTITIS EXTERNA ( Short note 2003)
A.k.a: Malignant Otitis Externa
DEFINITION:
Rare complication of Otitis Externa
Severe infection of temporal and adjacent bone
May lead to osteomyelitis of temporal bone and skull base
Commonly caused by Pseudomonas aeruginosa
Typically seen in immunocompromised and DM patients
COHEN DIAGNOSTIC CRITERIA:
| MAJOR:
|
MINOR:
|
| A- MicroAbscess | A – Age (elderly) |
| B- Bone scan positive | B – Bacterial culture (pseudomonas – 98%) |
| C- Cruciating pain | C – Cranial nerve palsy |
| D- Discharge | D – DM/ debilitating illness |
| E- Edema | E – ESR raised |
| G- Granulation tissue | |
| F- Failed medical therapy |
DIAGNOSIS:
Lab: ESR, swab c&s, HPE of granulation tissue, TWC, Glucose, Creatinine level
Imaging:
CT scan – to exclude temporal bone SCC. Findings: soft tissue enhancement in EAC +/- abscess
Technetium 99 – for diagnosis (absorbed by osteoclast and osteoblast)
Galium 67 – for prognosis (absorbed by macrophages)
TREATMENT:
Medical – IV abx (anti-pseudomonal): Ciprofloxacin 1/12, sugar control, pain control, ear toileting
Surgical – mastoidectomy + debridement of granulation tissue
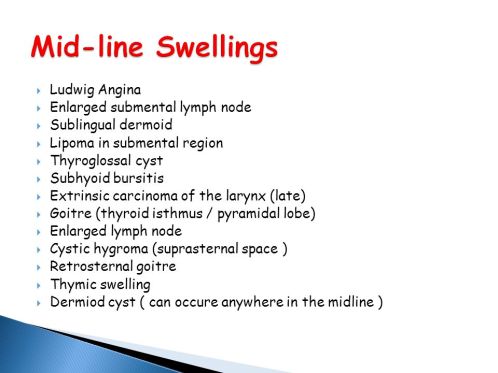
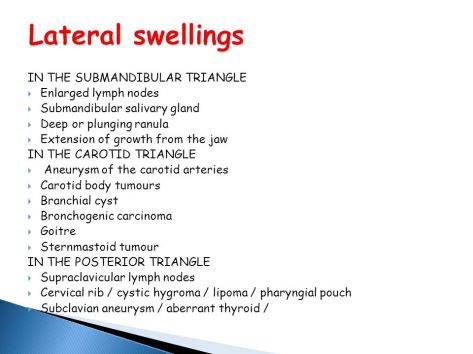
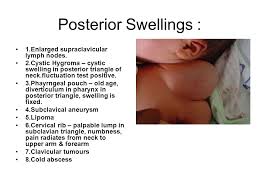
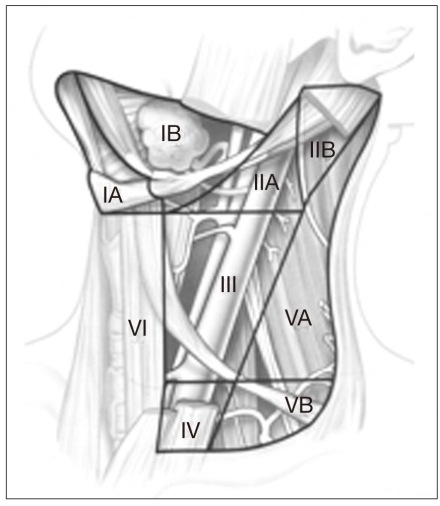
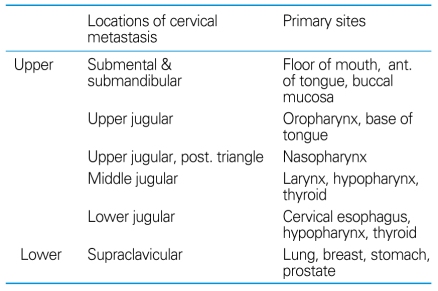
Neck mass – long case / short case
History:
- Site
- Duration
- Onset
- Progress
- Pain
- Secondary changes – ulceration/ discharge
- Aggravating factor
- Relieving factor
- Assoc symtoms: Dyspnea/ Dysphagia/ Trismus / Change of voice
- Fever
- URTI hx
- LOA / LOW
- H/o Trauma
- Any other swelling elsewhere
- Similar hx in the past
Examination:
Inspection:
- Number
- Site
- Size
- Shape
- Surface
- Edge
- Skin changes – colour / ulcer / punctum/ discharge/ necrotic patch
- Scar – transcervical / schobinger/ modified blair
- Trachea deviation
- Pulsatile
- Movement on deglutition
- Movement on protrusion of tongue
Palpation:
- Local rise of temperature
- Tenderness
- Confirm inspector findings – number / site/ size/ shape/ surface
- Consistency
- Mobility
- Fixity to overlying skin
- Pulsation – expansile/ transmitted


Relative Prevalence of Neck Mass Etiologies
| Type | Common | Uncommon | Rare |
|---|---|---|---|
|
|
|
— |
|
|
|
|
|
|
|
|
Reference:
1. Soo-Geun Wang. Differential Diagnosis and Treatment of Neck Masses. J Korean .Med Assoc. 2007 Jul;50(7):613-625.
Sudden Sensorineural Hearing Loss
- labyrinthitis
- autoimmune disease (eg: Cogan’s syndrome)
- Acoustic neuroma grows 1mm/year grow ,unilateral (bilateral in Type 2 Neurofibromatosis)
- Meningioma
- Vestibulotoxic: gentamicin(aminoglycoside), dietatic, aspirin, quinolone(antimalaria)
- Cochleotoxic: streptomycin, kanamycin,neomycin
- FBC – anemia, polycythemia, high twc
- ESR
- RP
- Fasting serum lipid
- FBS, HbA1c
- Autoimmune screening c3/4
- TFT -hypothyroid
- VDRL -syphilis
- PTA
- MRI- do later
- DM patient – monitor sugar as steroid started, vertigo, logistic —> treat in patient
- Others treat as outpatient
- inject dexamethasone through TM under LA (use EMLA) n lie down for 30 minutes- every week once for 3 weeks
- dose: 4 mg ( 1ml) each injection
- Age: Young <10 years old and >60 years old: bad
- Esr > 25: bad
- Vertigo: bad
- Comorbid: bad
- Severity: Severe to profound HL: bad, mild / moderate: good
- Bilateral: bad
- Tinnitus: good (protective)
Radiotherapy in Head and Neck Cancer
Complication of radiotherapy:
Early
- Skin – erythema, desquamation
- Mucosa – mucositis, dry mucosa
- Candidiasis
- Loss of appetite, nausea, vomitting ( Radiation sickness )
- Laryngeal edema
- Haematopoietic suppression
Late
- Skin – atrophy, fibrosis of subcutaneous tissue
- Xerostomia
- Eye – retinopathy, cataract
- Teeth – decay, osteoradionecrosis
- Trismus ( fibrosis of TMJ and muscles of mastication)
- Endocrine deficit – thyroid, pituitary
- Transverse myelitis
- Radiation induced malignancy – thyroid cancer, osteosarcoma
Why patients undergoing Radiotherapy need to have Hemoglobin level above 10g/dl?
- Low Hb —> low oxygen carrying capacity —> low oxygen —> less radiation-induced cytotoxic free radicals to kill the tumour cells
- Free radicals formation: O2 ——> O+ + O+
H2O ——> O+ + OH-
Is inappropiately high Hb good for radiotherapy?
- No. Increased blood viscosity —-> reduces tumour cell perfusion —–> less free radicals to kill the tumour cells