Rhinology
ENDOSCOPIC DACRYOCYSTORHINOSTOMY (EDCR)
Short Note 2003
Dacryocystorhinostomy:
Procedure whereby fistula of the lacrimal sac into the nasal cavity is created.
The operative approach to the sac may be external or endoscopic. The latter approach may use rigid telescopes or the microscope.
History:
Endonasal approach to correct nasolacrimal obstruction was described way back in 1800 by Caldwell, West and later during the begining of 1900 by Mosher.
McDonogh was the first to perform endoscopic dacryocystorhinostomy in 1989.
Indications:
- Socially unacceptable epiphora caused by anatomic or functional lacrimal sac or nasolacrimal duct obstruction
- Chronic dacryocystitis with purulent drainage from the canaliculi
- Inflammation of the skin overlying the lacrimal sac in the region of the medial canthus
- Dacryolith formation
- Benign lacrimal sac mass
Advantages of endoscopic DCR:
- better aesthetic result , no external scar.
- any concomittant intranasal pathology causing epiphora can be addressed
- avoids injury to the medial canthus and/or pathologic scar formation.
- preserves the pumping mechanism of the orbicularis oculi muscle.
- active infection of the lacrimal system is not a contraindication to surgery.
- It is especially superior to the external approach in revision surgery.
- less bloody than the external approach.
- the perioperative time is shorter.
- success rate is comparable to the external approach.
Disadvantages of endoscopic DCR:
- It requires specialized training in nasal endoscopic surgery.
- The endoscopic equipment is an expense.
Contraindications of endoscopic DCR:
– Presence of a firm indurated mass above the level
of medial canthus.
– Bloody epiphora
– Presence of bony destruction as seen in
radiological films
– Pseudoepiphora: is essentially reflux tearing: the
main gland over compensates secretion because
of lack of secretion from minor glands of along the
lid margin.
Surgery technique:
– Patient under GA
– Nasal packing with decongestants
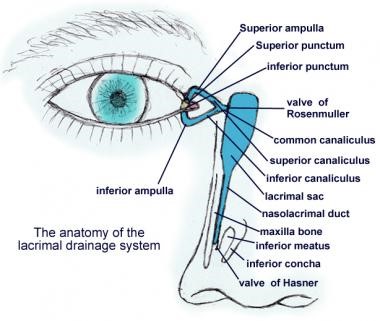
– Localisation of lacrimal sac: the anterior portion of middle turbinate, the sac lies just lateral to it. The lacrimal fossa is bounded by the anterior lacrimal crest, which consists of the frontal process of the maxillary bone. The posterior lacrimal crest is made up of the lacrimal bone itself.
– Mucosal incision: lateral wall mucosa is incised with a sickle knife and is elevated using a Freer elevator. The incision is made vertically from inferior to superior. After elevation the mucosa is removed using a Blakesley forceps.
– Bone removal: To expose the lacrimal sac, the bony lacrimal fossa must be uncovered first. Bone removal can be performed using a Kerrison’s punch forceps or by using a burr.
– Opening of lacrimal sac: After overlying bone removal the lacrimal sac can be incised using a sickle knife. An assistant could tent out the medial wall of the sac with lacrimal probes introduced through the canaliculi. The whole of the medial wall of the sac is removed.
– Topical mitomycin can be applied to the site of surgery to prevent restenosis of the sac.
JONES DYE TESTS
PRIMARY AND SECONDARY
Procedure
- Instil one drop of fluorescein into the conjunctival sac
- Put a cotton bud soaked in anaesthetic in the inferior meatus.
- If fluorescein is detected after five minutes, the system is patent (positive Primary Jones Test)
- If no fluorescein is discovered, this is a negative Primary Jones Test and the functional obstruction could be anywhere from the punctum to the Valve of Hasner.
- Next, wash the excess fluorescein from the conjunctival sac and syringe. If fluorescein is detected, then this shows it had entered the sac and constitutes a positive Secondary Jones Test and suggests a functional obstruction of the nasolacrimal duct.
- If no dye is found on the cotton bud after syringing, this is termed a negative Secondary Jones Test, because fluorescein had not entered the sac and, thus, there is stenosis of the puncta or canalicular system.
- If no saline appears in the nose, there is a complete obstruction somewhere in the lacrimal drainage system.
Hard stop
If the cannula touches the medial wall of the lacrimal sac and lacrimal bone, a definite end point is reached. It indicates that there is no complete obstruction in the canalicular system
Soft stop
If a spongy end point is felt, this indicates that the cannula has been prevented from entering the lacrimal sac. Therefore, there is a blockage in the canalicular system and there will be no distension of the lacrimal sac when the plunger is pressed.
Epistaxis
Causes of epistaxis MANAGEMENT
Local: ( T I 3N E A V D )
• Trauma
– Nose picking
– Facial injury
– Foreign body
• Idiopathic
• Inflammation
– Infection
– Allergic rhinosinusitis
– Nasal polyps
• Iatrogenic
– Surgery (for example, ENT/maxillofacial/ophthalmic)
– Nasal apparatus (for example, nasogastric tube)
• Neoplasia
– Benign (for example, juvenile angiofibroma)
– Malignant (for example, squamous cell carcinoma)
• Environmental:
– Dry cold conditions (presentations increase during winter
– Prolonged inhalation of dry air (Oxygen)
• Anatomical
– DNS/ septal spur
– Septal perforations
• Vascular
– Congenital (for example, hereditary haemorrhagic telangiectasia)
– Acquired (for example, Wegener’s granulomatosis)
• Drugs
– Nasal sprays (for example, topical decongestants)
– Abuse (for example, cocaine)
Systemic: (HO2D)
• Haematological
– Coagulopathies (for example, haemophilia)
– Thrombocytopenia (for example, leukaemia)
– Platelet dysfunction (for example, Von Willebrand’s disease)
• Organ failure
– Uraemia —> coagulopathy
– Liver (for example, cirrhosis) —> reduced vitamin K —> coagulopathy
• Drugs
– Anticoagulants (for example, heparin, warfarin)
– Antiplatelet (for example, aspirin, clopidogrel)
• Others
– Atherosclerosis
– Hypertension
MANAGEMENT
1. Attend immediately
2. Assess patient’s ABCDE
Airway:
• Risk of airway obstruction from blood in the posterior pharynx, or decreased level of consciousness from hypovolaemia.
Breathing:
• Assess depth of breathing and respiratory rate,
• Provide high flow oxygen via non rebreather mask
Circulation:
• Assess heart rate, blood pressure and capillary refill
• Insert x2 large bore IV, check HB, cross match blood, and start fluid resuscitation
Disability:
• Monitor patients level of consciousness this help determine the severity of haemorrhage
Exposure:
• Keep patient warm to prevent coagulopathy
• If epistaxis is caused by major trauma, always examine from for other injuries
For those not in extremis, use gold-standard first aid (also known as Trotter’s or Hippocratic method):
• Sit with head forward over a basin/sink
• Pinch the fleshy part of the nose (nares) firmly
• Hold the nose for 20 minutes without peeking
• Suck on some ice or place ice packs on the forehead or nape of neck
• Spit out any blood in the mouth: it is emetogenic
At the same time, get important history:
• Laterality, duration, frequency
• Severity, estimated blood loss
• Any contributing or inciting factors
• Family history or bleeding disorder
• Past medical history
• Current medications
Physical Examination:
• Site of bleeding: anterior or posterior
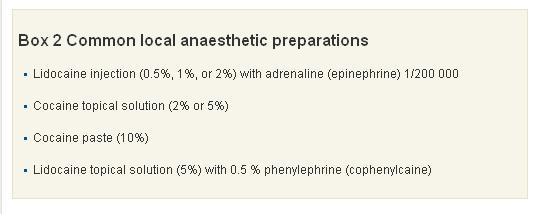
• Suctioning and application of topical local anaesthesia + vasoconstrictors to help with visualisation
• Gently insert Thudicum speculum and spread naris vertically. Use head light for good light source.
• A posterior source of bleeding is suggested by failure to visualise an anterior source, bleeding from both nares, and the visualisation of blood in the posterior pharynx.
Investigations:
• FBC – check haemoglobin level.
• GSH/ GXM
• PT/ INR- Coagulation studies are only of benefit in patients with a known coagulopathy or chronic liver disease, and should not be routine in patients presenting with epistaxis.
• Other bloods test should only be ordered if past medical history warrants further investigation (renal failure = U&E, chronic alcohol abuse = LFTs), and literature has shown they rarely change your management and add considerably to the cost of treating these patients.
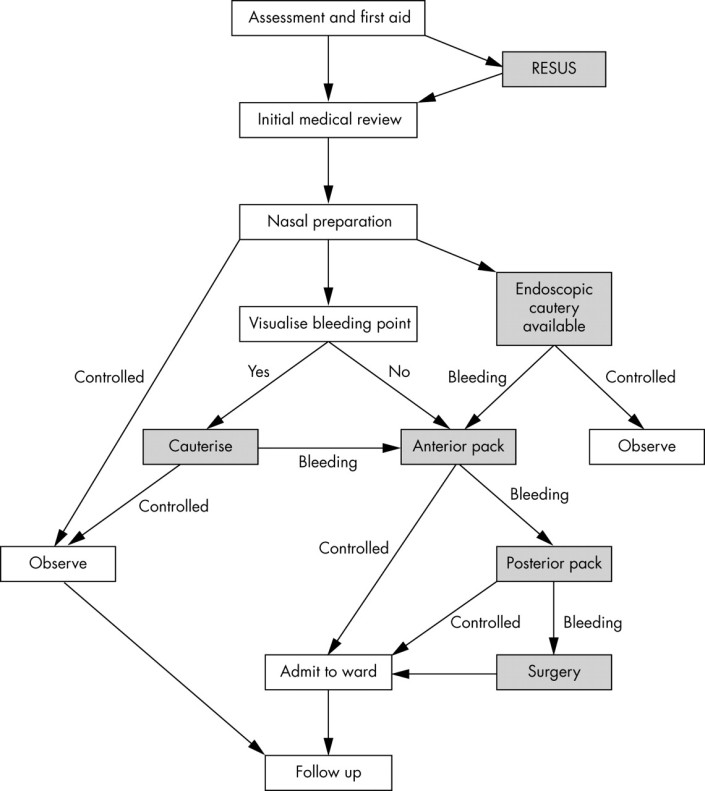
Cautery
1. Silver nitrate stick (75% silver nitrate, 25% potassium nitrate BP w/w): causing chemical damage to mucosal lining
– Careful removal of excess silver nitrate helps prevent staining of the vestibule or upper lip. If staining does occur, it should be neutralised immediately by applying normal saline.
– Only one side of the septum should be cauterised ( risk of septal perforation resulting from decreased vascularisation to the septal cartilage)
– Four to six week interval between cautery treatments to prevent septal perforation
2. Diathermy (Electrocautery)
– an electrical circuit that heats up a metal loop.
– thermal energy seals the bleeding vessel by radiation, not by direct contact
– complication: heat damage to the anterior nares and inferior turbinate.
Anterior packing
The nose should be packed if bleeding continues despite cautery or if no obvious bleeding is seen.
1. Merocel

Correct insertion of a nasal tampon (note that the direction is along the floor of the nasal cavity).
2. Rapid Rhino is an example of a carboxymethylcellulose pack. This is a hydrocolloid material, which acts as a platelet aggregator and also forms a lubricant on contact with water. Unlike Merocel, it has a cuff that is inflated by air and the hydrocolloid or Gel-Knit is supposed to preserve newly formed clot during removal.

3. Ribbon gauze. Pre-prepared packs eg: Vaseline or bismuth-iodoform paraffin paste impregnated packs.
If still bleeding:
Posterior packing
1. Foley catheter – use size 16 for adult
Inserted through the anterior nares and passed back until the tip is seen in the oropharynx. It is then inflated with 3–4 ml of water or air.
The catheter is pulled forward until the balloon engages the posterior choana. The nasal cavity is then packed anteriorly with ribbon gauze or a nasal sponge. The balloon is held firmly in place with an umbilical clamp at the anterior nares.
Protect the columella with a soft dressing, otherwise it is susceptible to pressure necrosis.
Other complications include posterior displacement of the balloon with potential airway compromise, deflation in situ (which is more likely to occur with air inflation) and rupture of the balloon, which when it contains water, could result in aspiration.
2. Brighton balloon
This is specifically manufactured for the treatment of epistaxis. It has a postnasal balloon and a mobile anterior balloon that are independently inflated.
 Sagittal view of the nasal cavity with a Brighton balloon in situ.
Sagittal view of the nasal cavity with a Brighton balloon in situ.

http://bestpractice.bmj.com/best-practice/monograph/421/treatment/step-by-step.html
- ADMIT WARD
- START ANTIBIOTIC – to prevent Toxic Shock Syndrome
- REMOVE PACKING AFTER 48 HOURS
- IF STILL BLEEDING, PACK AGAIN
- BRING PATIENT TO OT FOR EUA, KIV PROCEED
Surgery:
Diathermy
The localisation of a bleeding point under general anaesthetic is easier because of improved nasal access and instrumentation. The use of bipolar rather than monopolar diathermy is recommended, as there are reports of optic or oculomotor nerve damage.
Septal surgery
Septal surgery is sometimes performed to allow access to the nasal cavity. As most haemorrhages occur from the septum, raising a mucoperichondral flap during septal surgery can be beneficial as this will decrease blood flow to the mucosa, which often in itself stems bleeding. Surgery is also used to correct a deviated septum or remove a septal spur, which may be the cause of epistaxis. This occurs either by altering air flow through the nose or in severe cartilage deformities, by persistent mucosal irritation.
Sphenopalatine artery ligation
Anterior/posterior ethmoidal artery ligation
Internal maxillary artery ligation
The approach is a modified Caldwell-Luc operation, through the posterior wall of the maxillary sinus into the pterygopalatine fossa. The maxillary vessel can be either clipped or diathermied. Complications of this include devitalised gums and teeth, sinusitis, and problematic intraoperative bleeding.
External carotid artery ligation
Angiographic embolisation
Complications of nasal packing
• Toxic shock syndrome
• Blockage of
– nasolacrimal duct leading to epiphora
– sinus drainage leading to acute sinusitis
– nasal airway leading to hypoxia
• Nasovagal reflex: this reflex occurs during insertion of a pack or instrumentation of the nasal cavity. It leads to vagal stimulation, with consequent hypotension and bradycardia
• Sleep apnoea, attributable to decreased nasal air entry leading to hypoxia during somnolence
• Displacement of pack into oropharynx with risk of acute airway obstruction
References/ Sources:
1. http://lifeinthefastlane.com/epistaxis/
2. http://pmj.bmj.com/content/81/955/309.full
Sinus and Sinusitis – What are they?
Time and again, we always hear people interchangeably used these terms ‘sinus’ and ‘sinusitis’. Are they the same? What are they really are?
Definition:
Sinus aka Paranasal Sinuses = a group of four paired air -filled spaces in our skull.
There are 4 pairs, which are:
• The maxillary sinuses (the largest), in the cheekbones.
• The frontal sinuses, in the low-center of the forehead.
• The ethmoid sinuses, between the eyes, at the nasal bridge.
• The sphenoid sinuses, in bones behind the nasal cavity.
God created sinuses for few reasons. The biological roles are debatable, but a number of possible functions have been proposed:
• Decreasing the weight of the skull.
• Increasing resonance of the voice.
• Providing a buffer against facial trauma.
• Insulating sensitive structures like dental roots and eyes from rapid temperature fluctuations in the nasal cavity.
• Humidifying and heating of inhaled air because of slow air turnover in this region.
• Regulation of intranasal and serum gas pressures.
• Immunological defense
Sinus health depends on:
–Mucous secretion of normal viscosity, volume, and composition.
– Normal mucociliary flow to prevent mucous stasis and subsequent infection.
–Open sinus ostia to allow adequate drainage and aeration.
(Senior BA, Kennedy DW. Management of sinusitis in the asthmatic patient AAAI J,1996;77:6-19.)
Sinusitis is the term that refers to the inflammatory process involving one or more of the paranasal sinuses.
What causes sinusitis?
• colds
• bacterial upper respiratory tract infections
• fungal sinus infections
• allergies that cause mucus production in the sinuses
• lack of cilia motility, caused by disease (cilia are the small hairs located in your sinuses that move to push mucus out of your sinuses)
• nasal polyps or tumors
• deviated nasal septum
• enlarged or infected adenoids
• infected tooth (in rare cases bacteria can spread from the infected tooth to the sinuses)
• cystic fibrosis (a disease that causes thick, sticky mucus to build up in the body)
What are different classifications of sinusitis?
• Acute Sinusitis –signs and symptoms last longer than 10 days but less than 1 month
• Subacute sinusitis – signs and symptoms persist longer than 1month without improvement.
• Chronic sinusitis – signs and symptoms ast longer than 3 months.
• Recurrent – episodes lasting fewer than 1 months and separated by intervals of at least 10 days during which the patient is totally asymptomatic or 3 episodes in 6 months or 4/year



