Cordectomy
Cordectomy classification:
- Subepithelial cordectomy – resection of epithelium ( Type I)
- Subligamental cordectomy – resection of Reinke’s space and vocal ligament ( Type II )
- Transmuscular cordectomy – through vocalis muscle ( Type III )
- Total cordectomy ( Type IV )
- Extended cordectomy (Type V)
Va – encompasses anterior commissure and contralateral vocal folds
Vb – includes arythenoids
Vc – includes subglottis
Vd – includes ventricle
Tympanic membrane retraction
Tos classification of pars flaccida: (Tos et al)
- Grade I: Simple / slight retraction (not adhered to malleus)
- Grade II: Adhered to neck of malleus (fundus seen)
- Grade III: Hidden retraction pocket (fundus not seen)
- Grade IV: Erosion of scutum (outer attic wall)
Sade classification of pars tensa: (Sade et al)
- Grade I : Mild TM retraction
- Grade II : TM retraction in contact with incus or stapes (tympanoinducoplexy)
- Grade III : TM in contact with promontory wall (not adhered)
- Grade IV : TM adhered to promontory (atelectatic)
- Grade V : Type III or IV with TM perforation
VOCAL CORD PALSY / IMMOBILITY
VOCAL CORD PALSY / IMMOBILITY
Bilateral vocal fold (vocal cord) immobility (BVFI) is a broad term that refers to all forms of reduced or absent movement of the vocal folds.
Bilateral vocal fold (cord) paralysis (BVFP) refers to the neurologic causes of bilateral vocal fold immobility (BVFI) and specifically refers to the reduced or absent function of the vagus nerve or its distal branch, the recurrent laryngeal nerve (RLN).
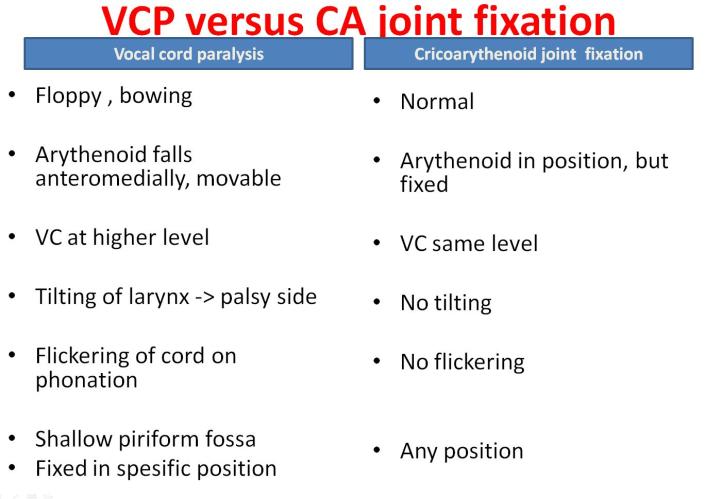
Vocal fold immobility may also result from mechanical derangement of the laryngeal structures, such as the cricoarytenoid (CA) joint.
What Are the Symptoms?
Both paresis and paralysis of voice box muscles result in:
Voice changes: Hoarseness; breathy voice; extra effort on speaking; excessive air pressure required to produce usual conversational voice; and diplophonia (voice sounds like a gargle).
Assess GRABAS score:
G rade (overall) of hoarseness
R ough
B reathy
A sthenic (weakness or lack of power in voice)
S trained
0=normal 1=slight 2=Moderate 3=Extreme
Airway problems: Shortness of breath with exertion, noisy breathing, and ineffective cough.
Swallowing problems: Aspiration symptoms – choking or coughing when swallowing food or drink. Cough with fever.
Also ask about reflux.
Classification
Laterality:
1. Unilateral vocal cord paralysis is most common.
2. Bilateral
Complete/ Incomplete
Incomplete paralysis
1. RLN palsy
Left (75%) , Right (15%) , BL (10%)
Abductor, adductor
2. Superior laryngeal nerve palsy
Cricothyroid muscles
Combine / complete paralysis
Causes
Systemic
Idiopathic
Localized caused
Supranuclear
Nuclear : nucleus ambigius
High vagal : combined lesion
Low vagal : RLN palsy
Central neurologic abnormalities
Causes bilateral vocal fold paralysis (BVFP)
Eg:
1. Arnold-Chiari deformity with meningomyelocele – the most common abnormality.
2. Other CNS insults (eg, infarct, craniotomy, asphyxia)
Aetiology: M2ATI3N
Malignant : (30% cases)
o Lung carcinoma 50%
o Esophageal carcinoma 20%
o Thyroid 10%
Iatrogenic:
o Thyroidectomy
o Esophagectomy
o Pneumonectomy
o CABG
Trauma:
o Penetrating neck or chest trauma.
o Post intubation
o Whiplash injuries
Neurological (5-10%)
o Poliomyelitis
o Multiple Sclerosis
o Myasthenia Gravis
o Guillian-Barre
o Wallenberg syndrome (lateral medullary stroke)
o Syringomyelia
o Encephalitis
o Parkinsons
o Diabetes Mellitus
o Ortner’s syndrome (left atrial hypertrophy)
Autoimmune:
o Rheumatoid arthritis – “fixed” cord
o Sarcoidosis
o Lupus
o Polyarteritis nodosa
Infectious:
o Syphilis
o Tuberculosis
o Thyroiditis
Idiopathic (20-25%): Viral causes ( viral neuritis usually on Right VC)
Medications
Vinca alkaloids – in children ungoing chemotherapy for lymphoma
o Vincristine and vinblastine
o Unilateral or bilateral
o Dose related
o Resolves with dose adjustment or cessation
SEMON’S LAW
Rosenbach(1880) & Semon (1881)
In all progressive organic lesions, abductor fibres of recurrent laryngeal nerve are more susceptible and thus first to be paralyzed compared to adductor fibres
• WHY ?
1. Nerve fibres supplying abductors are in periphery of RLN
2. Muscle bulk for the abductors is less, more susceptible
3. Phylogenetically, larynx main function is protection, so adductor function are maintained
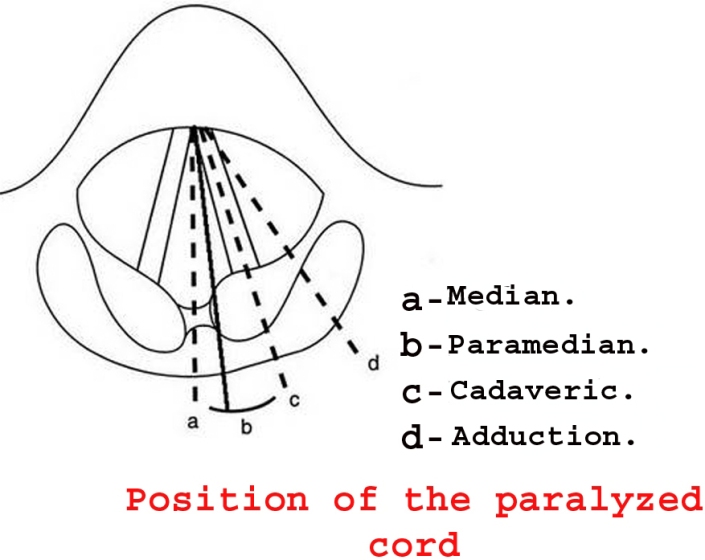
In progressive vocal cord palsy, vocal cord position will be in median or paramedian first, then later when the adductor fibres are also paralyzed, the vocal cord will be in cadaveric position.
Wegner and Grossman Theory : <popular theory>
• “In the absence of cricoarytenoid joint fixation, an immobile vocal cord in paramedian position has total pure unilateral recurrent nerve paralysis, and an immobile vocal cord in lateral position has a combined paralysis of superior and recurrent nerves (the adductive action of cricothyroid muscle is lost)”
• RLN palsy (intact SLN) – vocal cord in paramedian position (because cricoarythenoid adducts)
• RLN and SLN palsy – vocal cord in cadaveric position
Final position of paralysed VC is not static & determined by :
1. Vocal fold
– Length of VC
– Mass of VC
– Contour of VC
2. Muscle
– Atrophy
– Fibrosis
3. Nerve
– Synkinesis ( mass movement of all intrinsic muscles due to misinnervation)
– Reinnervation
4. Joint
– Ankylose
RELEVANT ANATOMY OF LARYNX
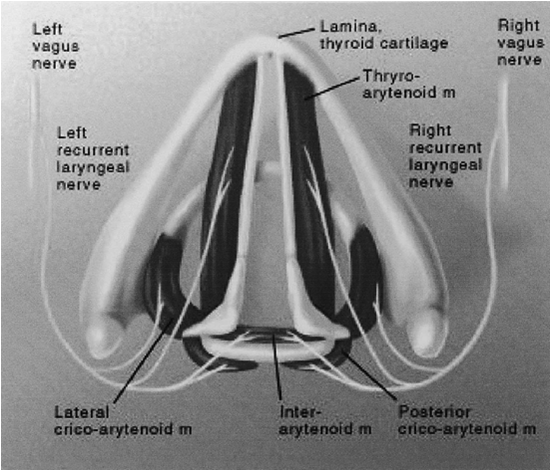
VAGUS NERVE
Larynx supplied by vagus nerve
The vagus nerve has three nuclei located within the medulla:
1. The nucleus ambiguus – the motor nucleus
2. The dorsal nucleus – innervate the involuntary muscles of the bronchi, esophagus, heart, stomach, small intestine, and part of the large intestine.
3. The nucleus of the tract of solitarius -carry sensory fibers from the pharynx, larynx, and esophagus.
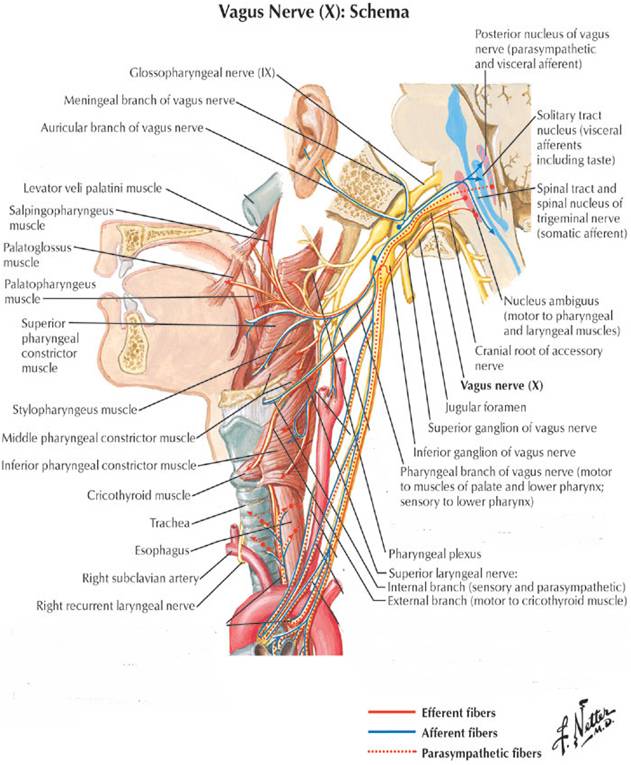
Upper motor neurons from cerebral cortex to nucleus ambiguus in the medulla
Lower motor neurons from nucleus ambiguus exit the medulla as the vagus nerve
Vagus nerve exits the skull base via the jugular foramen
Branches:
Pharyngeal branch
Superior laryngeal nerve
Recurrent laryngeal nerve
Superior laryngeal nerve
1. Internal branch – pierce thyrohyoid membrane to supply sensation of larynx above the VC
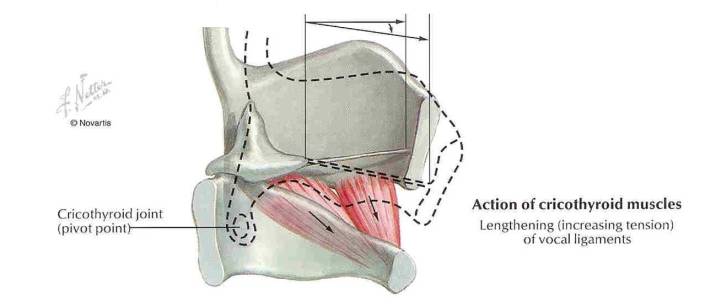
2. External branch –at the upper pole of thyroid gland and supply cricothyroid muscle ( the tensor of VC which controls vocal fold lengthening and pitch)
Recurrent laryngeal nerve
• Left – arches around arch of aorta lateral to liagmentum arteriosum, then nters TE groove
• Right –arches around Right subclavian artery, then enter TE groove at 45 degree angle
• Behr’s triangle:
superior: inferior thyroid artery
lateral: common carotid artery
medial: recurrent laryngeal nerve
• Enters the larynx beneath the cricopharyngeal muscle
• Motor supply to all intrinsic muscles of the larynx except cricothyroid and sensory supply to larynx below VC
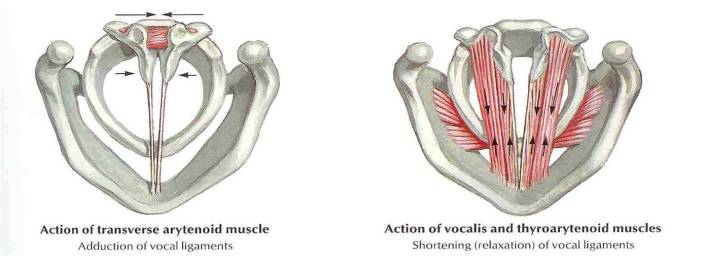
MUSCLES OF THE LARYNX
1. Cricothyroid
2. Posterior cricoarythenoid
3. Lateral cricoarythenoid
4. Transverse arythenoid
5. Oblique arythenoid
6. Thyroarythenoid (vocalis)
Epistaxis
Causes of epistaxis MANAGEMENT
Local: ( T I 3N E A V D )
• Trauma
– Nose picking
– Facial injury
– Foreign body
• Idiopathic
• Inflammation
– Infection
– Allergic rhinosinusitis
– Nasal polyps
• Iatrogenic
– Surgery (for example, ENT/maxillofacial/ophthalmic)
– Nasal apparatus (for example, nasogastric tube)
• Neoplasia
– Benign (for example, juvenile angiofibroma)
– Malignant (for example, squamous cell carcinoma)
• Environmental:
– Dry cold conditions (presentations increase during winter
– Prolonged inhalation of dry air (Oxygen)
• Anatomical
– DNS/ septal spur
– Septal perforations
• Vascular
– Congenital (for example, hereditary haemorrhagic telangiectasia)
– Acquired (for example, Wegener’s granulomatosis)
• Drugs
– Nasal sprays (for example, topical decongestants)
– Abuse (for example, cocaine)
Systemic: (HO2D)
• Haematological
– Coagulopathies (for example, haemophilia)
– Thrombocytopenia (for example, leukaemia)
– Platelet dysfunction (for example, Von Willebrand’s disease)
• Organ failure
– Uraemia —> coagulopathy
– Liver (for example, cirrhosis) —> reduced vitamin K —> coagulopathy
• Drugs
– Anticoagulants (for example, heparin, warfarin)
– Antiplatelet (for example, aspirin, clopidogrel)
• Others
– Atherosclerosis
– Hypertension
MANAGEMENT
1. Attend immediately
2. Assess patient’s ABCDE
Airway:
• Risk of airway obstruction from blood in the posterior pharynx, or decreased level of consciousness from hypovolaemia.
Breathing:
• Assess depth of breathing and respiratory rate,
• Provide high flow oxygen via non rebreather mask
Circulation:
• Assess heart rate, blood pressure and capillary refill
• Insert x2 large bore IV, check HB, cross match blood, and start fluid resuscitation
Disability:
• Monitor patients level of consciousness this help determine the severity of haemorrhage
Exposure:
• Keep patient warm to prevent coagulopathy
• If epistaxis is caused by major trauma, always examine from for other injuries
For those not in extremis, use gold-standard first aid (also known as Trotter’s or Hippocratic method):
• Sit with head forward over a basin/sink
• Pinch the fleshy part of the nose (nares) firmly
• Hold the nose for 20 minutes without peeking
• Suck on some ice or place ice packs on the forehead or nape of neck
• Spit out any blood in the mouth: it is emetogenic
At the same time, get important history:
• Laterality, duration, frequency
• Severity, estimated blood loss
• Any contributing or inciting factors
• Family history or bleeding disorder
• Past medical history
• Current medications
Physical Examination:
• Site of bleeding: anterior or posterior
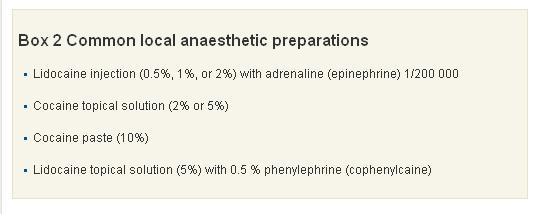
• Suctioning and application of topical local anaesthesia + vasoconstrictors to help with visualisation
• Gently insert Thudicum speculum and spread naris vertically. Use head light for good light source.
• A posterior source of bleeding is suggested by failure to visualise an anterior source, bleeding from both nares, and the visualisation of blood in the posterior pharynx.
Investigations:
• FBC – check haemoglobin level.
• GSH/ GXM
• PT/ INR- Coagulation studies are only of benefit in patients with a known coagulopathy or chronic liver disease, and should not be routine in patients presenting with epistaxis.
• Other bloods test should only be ordered if past medical history warrants further investigation (renal failure = U&E, chronic alcohol abuse = LFTs), and literature has shown they rarely change your management and add considerably to the cost of treating these patients.
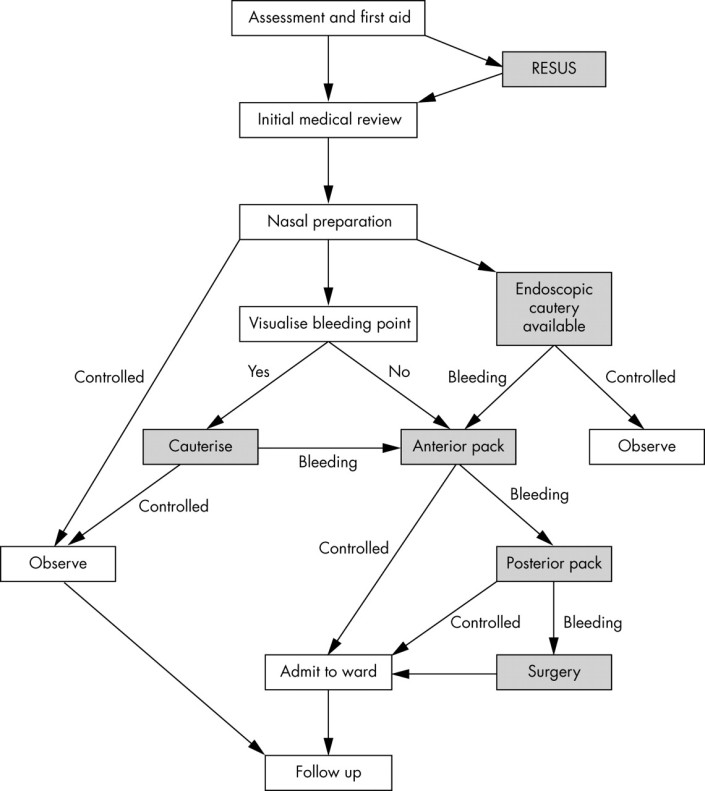
Cautery
1. Silver nitrate stick (75% silver nitrate, 25% potassium nitrate BP w/w): causing chemical damage to mucosal lining
– Careful removal of excess silver nitrate helps prevent staining of the vestibule or upper lip. If staining does occur, it should be neutralised immediately by applying normal saline.
– Only one side of the septum should be cauterised ( risk of septal perforation resulting from decreased vascularisation to the septal cartilage)
– Four to six week interval between cautery treatments to prevent septal perforation
2. Diathermy (Electrocautery)
– an electrical circuit that heats up a metal loop.
– thermal energy seals the bleeding vessel by radiation, not by direct contact
– complication: heat damage to the anterior nares and inferior turbinate.
Anterior packing
The nose should be packed if bleeding continues despite cautery or if no obvious bleeding is seen.
1. Merocel

Correct insertion of a nasal tampon (note that the direction is along the floor of the nasal cavity).
2. Rapid Rhino is an example of a carboxymethylcellulose pack. This is a hydrocolloid material, which acts as a platelet aggregator and also forms a lubricant on contact with water. Unlike Merocel, it has a cuff that is inflated by air and the hydrocolloid or Gel-Knit is supposed to preserve newly formed clot during removal.

3. Ribbon gauze. Pre-prepared packs eg: Vaseline or bismuth-iodoform paraffin paste impregnated packs.
If still bleeding:
Posterior packing
1. Foley catheter – use size 16 for adult
Inserted through the anterior nares and passed back until the tip is seen in the oropharynx. It is then inflated with 3–4 ml of water or air.
The catheter is pulled forward until the balloon engages the posterior choana. The nasal cavity is then packed anteriorly with ribbon gauze or a nasal sponge. The balloon is held firmly in place with an umbilical clamp at the anterior nares.
Protect the columella with a soft dressing, otherwise it is susceptible to pressure necrosis.
Other complications include posterior displacement of the balloon with potential airway compromise, deflation in situ (which is more likely to occur with air inflation) and rupture of the balloon, which when it contains water, could result in aspiration.
2. Brighton balloon
This is specifically manufactured for the treatment of epistaxis. It has a postnasal balloon and a mobile anterior balloon that are independently inflated.
 Sagittal view of the nasal cavity with a Brighton balloon in situ.
Sagittal view of the nasal cavity with a Brighton balloon in situ.

http://bestpractice.bmj.com/best-practice/monograph/421/treatment/step-by-step.html
- ADMIT WARD
- START ANTIBIOTIC – to prevent Toxic Shock Syndrome
- REMOVE PACKING AFTER 48 HOURS
- IF STILL BLEEDING, PACK AGAIN
- BRING PATIENT TO OT FOR EUA, KIV PROCEED
Surgery:
Diathermy
The localisation of a bleeding point under general anaesthetic is easier because of improved nasal access and instrumentation. The use of bipolar rather than monopolar diathermy is recommended, as there are reports of optic or oculomotor nerve damage.
Septal surgery
Septal surgery is sometimes performed to allow access to the nasal cavity. As most haemorrhages occur from the septum, raising a mucoperichondral flap during septal surgery can be beneficial as this will decrease blood flow to the mucosa, which often in itself stems bleeding. Surgery is also used to correct a deviated septum or remove a septal spur, which may be the cause of epistaxis. This occurs either by altering air flow through the nose or in severe cartilage deformities, by persistent mucosal irritation.
Sphenopalatine artery ligation
Anterior/posterior ethmoidal artery ligation
Internal maxillary artery ligation
The approach is a modified Caldwell-Luc operation, through the posterior wall of the maxillary sinus into the pterygopalatine fossa. The maxillary vessel can be either clipped or diathermied. Complications of this include devitalised gums and teeth, sinusitis, and problematic intraoperative bleeding.
External carotid artery ligation
Angiographic embolisation
Complications of nasal packing
• Toxic shock syndrome
• Blockage of
– nasolacrimal duct leading to epiphora
– sinus drainage leading to acute sinusitis
– nasal airway leading to hypoxia
• Nasovagal reflex: this reflex occurs during insertion of a pack or instrumentation of the nasal cavity. It leads to vagal stimulation, with consequent hypotension and bradycardia
• Sleep apnoea, attributable to decreased nasal air entry leading to hypoxia during somnolence
• Displacement of pack into oropharynx with risk of acute airway obstruction
References/ Sources:
1. http://lifeinthefastlane.com/epistaxis/
2. http://pmj.bmj.com/content/81/955/309.full
Tonsillectomy
Blood supply & relation of tonsils:
Tonsillectomy:
Surgical procedure that completely removes the tonsil, including its capsule by dissecting the peritonsillar space between the tonsil capsule and the muscular wall.
Indication for tonsillectomy:
- Recurrent infections of throat: (typically group A betahemolytic streptococcal)
- 7 or more episodes in 1 year
- 5 or more episodes per year in 2 years
- 3 or more episodes per year in 3 years
- 2 weeks or more of lost of school or work in a year
2. Peritonsillar abscess
- Children: 4-6 weeks after the 1st episode
- Adult: after 2nd episode
3. Tonsillitis causing febrile seizure
4. Tonsillar hypertrophy causing airway obstruction (OSA)
5. Suspicion of malignancy eg unilateral tonsillar hypertrophy eg: extranodal intratonsillar lymphoma, SCC tonsil
6. Chronic tonsillitis
Complications:
Early:
- Primary hemorrhage (at time to surgery)
- Reactionary hemorrhage (within 48hours post op) because a clot in a vessel has been displaced, or a ligature has slipped.
- Injury to tonsillar pillars, uvula, soft palate, tongue, teeth
- Aspiration (prevention: throat pack)
- Difficult intubation causing laryngospasm, laryngeal edema
Late:
- Pain
- Secondary hemorrhage – 8 to 14 days later when the wound has become infected and eroded a vessel.
- Infection
- Altered taste (dysgeusia)- due to injury to glossopharyngeal nerve
- Referred otalgia
Unusual complications:
- Necrotizing fasciitis
- Surgical emphysema due to injury to superior contrictor muscle
- Velopharyngeal insufficiency
- Hemotoma at lingual / BOT
- Mediastinitis
- Atlantoaxial subluxation
Intraoperatively if you encounter bleeding, how do you stop the bleeding?
- Tonsillar square with or without adrenaline to give compression and pack the area
- Coagulate or cauterize using bipolar diathermy
- Tie ~ use Burkitt artery forcep and then tie
Management for unilateral tonsil enlargement:
Assess:
- Size
- Appearance
- Neck nodes/ swelling
- Constitutional symptoms
- Pain
- Bleeding
If suspicious of malignancy – do tonsillectomy
If not, give 1 course of antibiotic and reassess.
Causes for unilateral tonsillar enlargement:
Divided into: anatomical variation, infective and neoplasm
Neoplasm
- Lymphoma
- SCC
Infective
- Tuberculosis
- Actinomycosis
- Paratonsillar abscess or peritonsillitis pushing tonsil medially
Anatomical variations
- asymmetrical tonsillar depth or tonsillar pillars
Stroboscopy
What is videostroboscopy?
It is a method used for viewing and recording the vocal cord vibration and mucosal wave whereby digital computer and strobe light are used to make the images of the vocal cord vibrations appear in slow motion, so that any abnormal patterns of vibration may be detected.
What are the advantages of videostroboscopy?
- The vibrations of the vocal cords are much too rapid to be observed by the unaided eye under a regular light source. Stroboscopy provides illumination of the larynx with quick pulses of light, which allows for detailed assessment of vocal cord movement in terms of vocal cord movement
- Helps the speech pathologist, physician and patient to obtain a better understanding of the way the vocal folds are functioning, and develop a specific treatment plan.
- The information acquired from the stroboscopic examination of the vocal folds is essential for planning effective phonomicrosurgery (endoscopic surgery to enhance vocal function).
- Structural or tissue abnormalities may be detected as well.
- If a repeat videostroboscopy is needed at a later date, the results can be compared to the previous exam. This allows the voice care team to evaluate the patient’s progress.
- Formal reports, still photos and portions of the video examination can be provided to the patient.
Procedure:
The procedure itself lasts for just 10-15 minutes. A rigid telescope is placed into the mouth OR a small flexible telescope is placed into the nose. The scope will be in the mouth or nose for just a brief time (no longer than 1 minute at a time, usually), and you will always be able to breathe during the test. You will be asked to say various sounds, and a video of the vocal cords will be displayed on a television monitor. (The recording will be replayed later)
Sedation:
A light spray of topical anesthetic may be used if needed, but there is no sedation necessary. The anesthetic is sweet-tasting, and usually wears off in about 15-20 minutes. There is no need to arrange for someone to drive you to and from the appointment.
(Referance: http://www.ent-stl.com/)
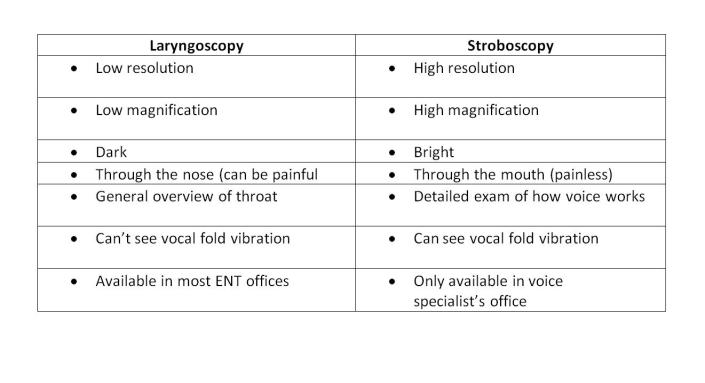
What is the difference between laryngoscopy and stroboscopy?
Info from: http://www.ohniww.org/
It it is critical in cases of voice problems to have a stroboscopy to accurately diagnose and treat your voice problem.
Links for video stroboscopy:
https://www.youtube.com/watch?v=mJedwz_r2Pc
Laryngeal surgery
Classification of laryngeal surgery:
Divided into endoscopic and open techniques. Open techniques divided into expansion and resection.
- Endoscopic:
- Dilatation – bougie, balloon
- LASER: shapshay
- Cold instrumentation
- Open:
Expansion:
- LTR
- Anterior split
- Posterior split
- Antero posterior split
Put costal cartilage graft for expansion or tracheal mucosal flap
Resection:
- Cricotracheal resection (CTR)
- Tracheal resection and anastomoses (TRA)
- Cricotracheal resection and anastomoses (CTRA)
T tube
Why T tube is better than Shilley tube?
- Self cleansing
- Stent the upper limb of segment
Immediate Complications of Post Operative TRA
- Anastomotic leak —> subcutaneous emphysema
- Hematoma
- Pneumon
- Local infection – SSI, hemorrhage
- DVT
Other complications:
- Recurrent stenosis
- Laryngeal dysfunction causing VC palsy (50% temporary)
Contraindications of TRA:
- Less than 1cm from VC (in children between 3mm to 5mm)
- Length of stenosis >4cm (must have adequate trachea for anastomoses)
- Tracheomalacia
- Multilevel stenosis
- Previous RT
- Failed larynhotracheal reconstruction before
- Poor pulmonary function – assess single breath counting, PEFR, FEV1
- Debilitating medical illnesses- COAD, uncontrolled DM
- Vocal cord immobility
Prognosis of surgery depends on:
- Age
- Comorbid
- Site of stenosis: Subglottic stenosis, trachea stenosis
- Grade of obstruction – CM grading
- Length of stenosis
- Tracheomalacia
- Presence of tracheostomy at time to resection
- Presence of 2′ airway pathology
- VC – normal mobility or impaired
- Obese, thick neck, neck circumference —> increase complications
Stenting in larynx:
- Stable larynx ie: expansion with anterior graft doesn’t need stent
- Unstable larynx ie: expansion with anteroposterior graft needs stent
- Stent causes granulation tissue so must aim to take out by 6 weeks
- Types of stents: Rubber stent, LTMOLD stent
Bougie vs Balloon dilatation:
Bougie:
- Free , not costly
- Shearing force –> increase reformation of stenosis due to scarring ( not good)
Balloon: RM1k ++
- Expensive
- Radial force –> less epithelial injury, less scar contraction (good)
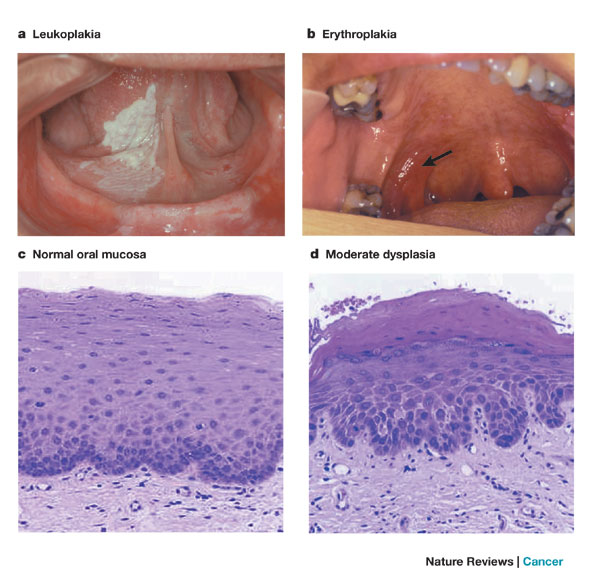
Leukoplakia
Definition of Leukoplakia:
- Premalignant condition
- Characterised by a white patch or plaque that cannot be characterized clinically or histologically as any other disease. (WHO Definition)
How does Verrucous Carcinoma differ from SCC?
Verrucous Carcinoma: “Ackerman’s tumor.” – 1st described by Ackerman
- Uncommon variant of SCC, locally aggressive, clinically exophytic, low-grade, slow-growing, well-differentiated squamous cell carcinoma with minimal metastatic potential.
- Risk factors: tobacco chewing, oral snuff “Snuff dipper’s cancer”, smoking, alcohol, betel nut chewing
- Good prognosis. Local recurrence is not uncommon, but metastasis to distant parts of the body is rare.
- Painless, thick white plaque resembling a cauliflower (warty lesion)
- Commonest site: Oral cavity
- Treatment: Wide local excision or radiotherapy
Post work durian treat from the big boss
First and foremost I would like to congratulate all of my PPUKM kakaks and abangs who have passed their part 2 exam. 100% pass woohoo!!
Alhamdulillah. They have done so well and I can’t help but feeling so proud of them. Hopefully when my time comes, I will perform as good as them.
Anyway, as a selingan, my big boss is obviously in happy mood these past few days (maybe because his students have been performing well in exams?) and….. Also, there’s a last minute cancellation on one of his operation cases due to some reasons that I of course can’t mention here. So, since we had time to fill in, the generous big boss decided to bring us out for a durian treat outing!
Hehe. Yeay *happy dance*
P/s: If you don’t eat durian, you are missing one of the best things in the world. I’m serious.
- ← Previous
- 1
- 2
- 3
- 4
- Next →