CAVERNOUS SINUS THROMBOSIS
Short Note 2003
DEFINITION:
- Formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains deoxygenated blood from the brain back to the heart.
ETIOLOGY:
Usually from a spreading infection in the nose, sinuses, ears, or teeth.
Nasal furuncle (50%), sphenoidal or ethmoidal sinuses (30%) and dental infections (10%).
Less common primary sites of infection include tonsils, soft palate, middle ear, or orbit (orbital cellulitis).
The highly anastomotic venous system of the paranasal sinuses allows retrograde spread of infection to the cavernous sinus via the superior and inferior ophthalmic veins (valveless veins).
Causative organism: Staphylococcus infectious 70% of the cases. Streptococcus is the second leading cause. Gram-negative rods and anaerobes, rarely Aspergillus fumigatus and mucormycosis.
CLINICAL FEATURES:
-abrupt onset of unilateral periorbital edema, headache,
photophobia and proptosis
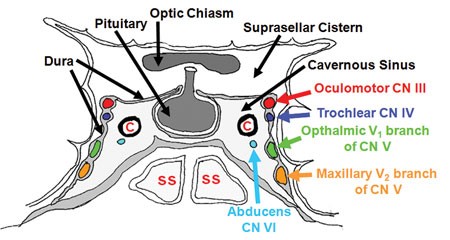
– Ptosis, chemosis, cranial nerve palsies (III, IV, V,VI).
Sixth nerve palsy is the most common. ( it is the content of cavernous sinus while others are located at lateral wall)
– Sensory deficits of the ophthalmic and maxillary branch of the fifth nerve are common.
– Periorbital sensory loss and impaired corneal reflex
– Papilledema, retinal hemorrhages, and decreased visual acuity and blindness may occur from venous – congestion within the retina.
– Fever, tachycardia and sepsis may be present.
– Headache with nuchal rigidity may occur.
– Pupil may be dilated and sluggishly reactive.
– Infection can spread to contralateral cavernous sinus within 24–48 hours of initial presentation.
INVESTIGATIONS:
FBC, ESR, blood cultures, and sinus cultures
Lumbar puncture TRO meningitis.
CT BRAIN/ PNS: Opacification, sclerosis, and air-fluid levels, thickening of the superior ophthalmic vein, and irregular filling defects within the cavernous sinus.
MRI, MR venogram : more sensitive than a CT scan & imaging studies of choice. Findings may include deformity of the internal carotid artery within the cavernous sinus, and an obvious signal hyperintensity within thrombosed vascular sinuses on all pulse sequences.
TREATMENT:
Medical:
- IV Antibiotics: IV Rocephine 2g OD
+/- IV Metronidazole 500mg TDS
- Anticoagulation with heparin is controversial.
- Steroid therapy is also controversial.
Surgical drainage with sphenoidotomy is indicated if the primary site of infection is thought to be the sphenoidal sinuses.
All patients with CST are usually treated with prolonged courses (3–4 weeks) of IV antibiotics. If there is evidence of complications such as intracranial suppuration, 6–8 weeks of total therapy may be warranted.

January 7, 2016 at 12:58 am
Assalamualaikum doc. Recently. Saya join kem selama sebulan. Dan peserta berumur dari 7 tahun – 17 tahun. 🙂 saya as a fasi. Dan person in charge unit rawatan. Ada dua org adik ni ( peserta lelaki) yang A tu berumur dlm lingkungan 11 tahun. Hidung dia asyik berdarah, dia demam juga. Bawak p klinik doc bagi ubat utk demam. And ckap dia panas dalam. Setelah 3 hari dia dibenarkan balik rumah sbab keadaan dia mmbimbangkan. Jd lebih baikkan if parent dia yg uruskan. Yang B ni keadaan sama hidung berdarah. Tpi lagi banyak. Dan lbih kerap kalau dlm Sehari tu dlm 5 Kali cmtu, demam juga tapi sekejap sahaja. Utk yg A dia first time hidung berdarah. Utk yg B pun sama dan B berumur 8 tahun. Adakah normal budak2 lelaki hidung berdarah.?
LikeLike