Rhinology
ENDOSCOPIC DACRYOCYSTORHINOSTOMY (EDCR)
Short Note 2003
Dacryocystorhinostomy:
Procedure whereby fistula of the lacrimal sac into the nasal cavity is created.
The operative approach to the sac may be external or endoscopic. The latter approach may use rigid telescopes or the microscope.
History:
Endonasal approach to correct nasolacrimal obstruction was described way back in 1800 by Caldwell, West and later during the begining of 1900 by Mosher.
McDonogh was the first to perform endoscopic dacryocystorhinostomy in 1989.
Indications:
- Socially unacceptable epiphora caused by anatomic or functional lacrimal sac or nasolacrimal duct obstruction
- Chronic dacryocystitis with purulent drainage from the canaliculi
- Inflammation of the skin overlying the lacrimal sac in the region of the medial canthus
- Dacryolith formation
- Benign lacrimal sac mass
Advantages of endoscopic DCR:
- better aesthetic result , no external scar.
- any concomittant intranasal pathology causing epiphora can be addressed
- avoids injury to the medial canthus and/or pathologic scar formation.
- preserves the pumping mechanism of the orbicularis oculi muscle.
- active infection of the lacrimal system is not a contraindication to surgery.
- It is especially superior to the external approach in revision surgery.
- less bloody than the external approach.
- the perioperative time is shorter.
- success rate is comparable to the external approach.
Disadvantages of endoscopic DCR:
- It requires specialized training in nasal endoscopic surgery.
- The endoscopic equipment is an expense.
Contraindications of endoscopic DCR:
– Presence of a firm indurated mass above the level
of medial canthus.
– Bloody epiphora
– Presence of bony destruction as seen in
radiological films
– Pseudoepiphora: is essentially reflux tearing: the
main gland over compensates secretion because
of lack of secretion from minor glands of along the
lid margin.
Surgery technique:
– Patient under GA
– Nasal packing with decongestants
– Localisation of lacrimal sac: the anterior portion of middle turbinate, the sac lies just lateral to it. The lacrimal fossa is bounded by the anterior lacrimal crest, which consists of the frontal process of the maxillary bone. The posterior lacrimal crest is made up of the lacrimal bone itself.
– Mucosal incision: lateral wall mucosa is incised with a sickle knife and is elevated using a Freer elevator. The incision is made vertically from inferior to superior. After elevation the mucosa is removed using a Blakesley forceps.
– Bone removal: To expose the lacrimal sac, the bony lacrimal fossa must be uncovered first. Bone removal can be performed using a Kerrison’s punch forceps or by using a burr.
– Opening of lacrimal sac: After overlying bone removal the lacrimal sac can be incised using a sickle knife. An assistant could tent out the medial wall of the sac with lacrimal probes introduced through the canaliculi. The whole of the medial wall of the sac is removed.
– Topical mitomycin can be applied to the site of surgery to prevent restenosis of the sac.
JONES DYE TESTS
PRIMARY AND SECONDARY
Procedure
- Instil one drop of fluorescein into the conjunctival sac
- Put a cotton bud soaked in anaesthetic in the inferior meatus.
- If fluorescein is detected after five minutes, the system is patent (positive Primary Jones Test)
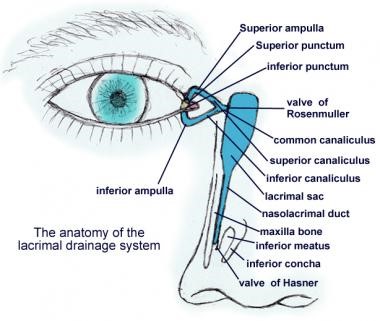
- If no fluorescein is discovered, this is a negative Primary Jones Test and the functional obstruction could be anywhere from the punctum to the Valve of Hasner.
- Next, wash the excess fluorescein from the conjunctival sac and syringe. If fluorescein is detected, then this shows it had entered the sac and constitutes a positive Secondary Jones Test and suggests a functional obstruction of the nasolacrimal duct.
- If no dye is found on the cotton bud after syringing, this is termed a negative Secondary Jones Test, because fluorescein had not entered the sac and, thus, there is stenosis of the puncta or canalicular system.
- If no saline appears in the nose, there is a complete obstruction somewhere in the lacrimal drainage system.
Hard stop
If the cannula touches the medial wall of the lacrimal sac and lacrimal bone, a definite end point is reached. It indicates that there is no complete obstruction in the canalicular system
Soft stop
If a spongy end point is felt, this indicates that the cannula has been prevented from entering the lacrimal sac. Therefore, there is a blockage in the canalicular system and there will be no distension of the lacrimal sac when the plunger is pressed.